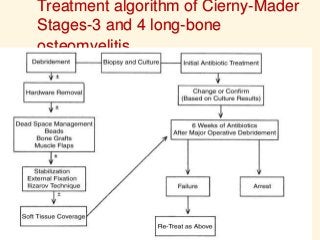
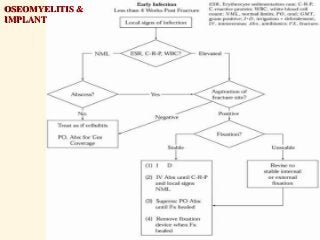
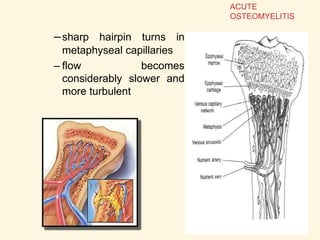
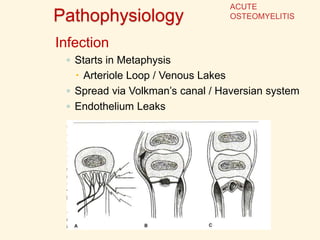
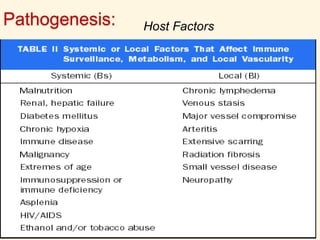
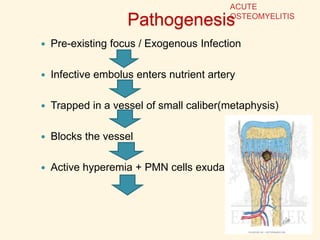
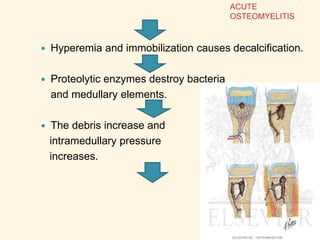
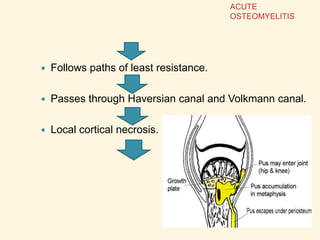
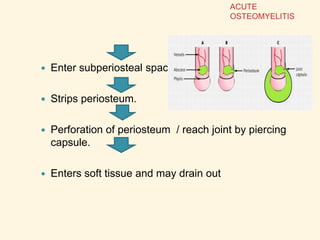
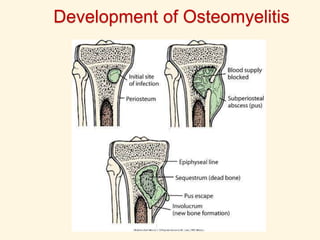
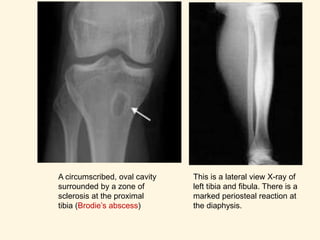
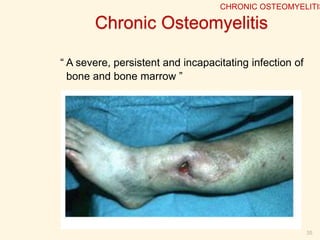
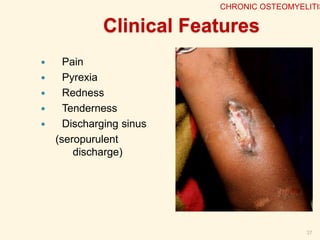
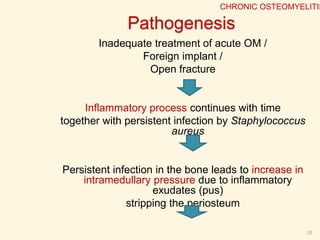
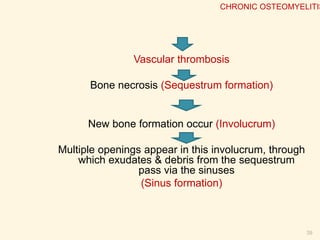
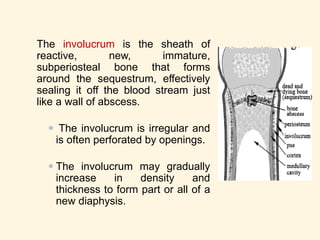
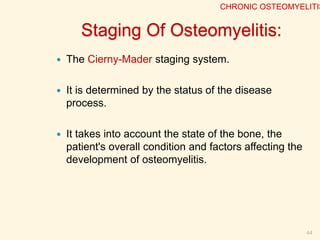
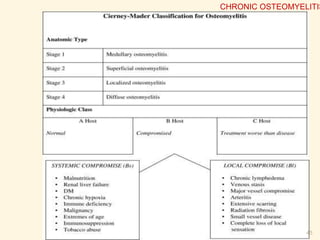
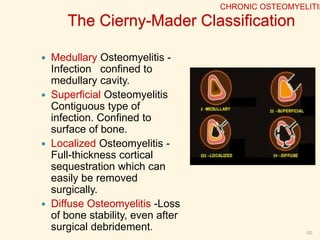
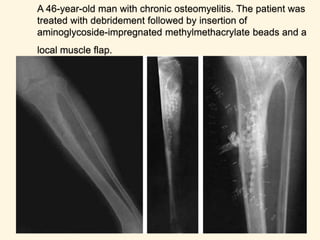
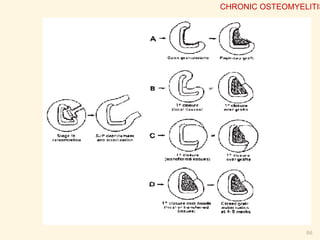
Osteomyelitis is an inflammatory process of bone caused by microbial infection. It can be acute, subacute, or chronic depending on duration. Common causes include hematogenous spread from other infections as well as direct introduction through open fractures or wounds. In acute osteomyelitis, infection starts in the metaphysis and can spread through bone canals, potentially crossing the growth plate in children. Chronic osteomyelitis results from inadequate treatment of acute infection and is characterized by persistent infection, bone necrosis, and sinus tract formation. Staging systems help classify osteomyelitis based on extent of bone and soft tissue involvement.












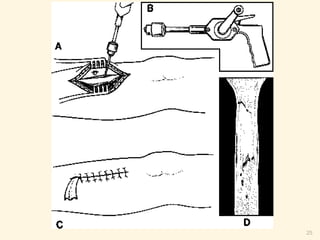






















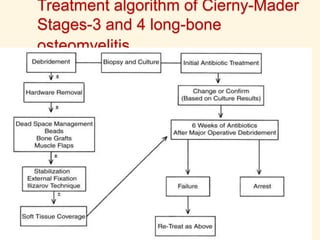
![- Antibiotic (IV route) is given for 10 days prior to
surgery.
- After the major debridement surgery, antibiotic is
continued for another 6 weeks (min) but usually
>3months.
[treat until inflammatory parameters (ESR) are
normal]
67
CHRONIC OSTEOMYELITIS](https://image.slidesharecdn.com/osteomyelitis-140627001957-phpapp02/85/Osteomyelitis-67-320.jpg)