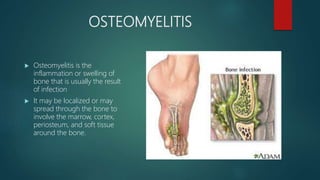
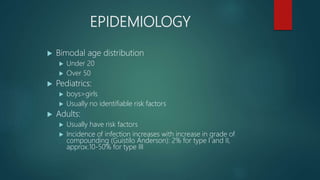
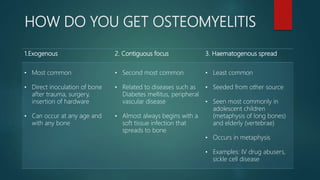
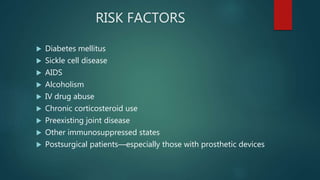
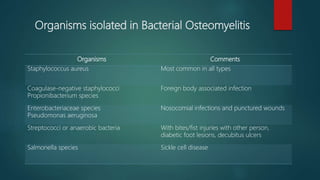
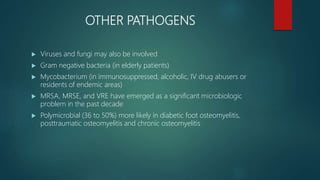
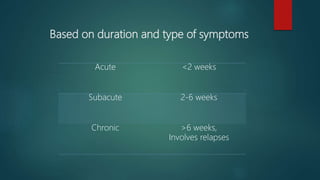
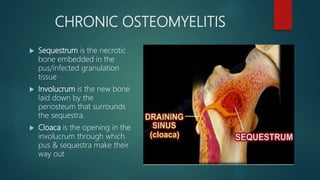
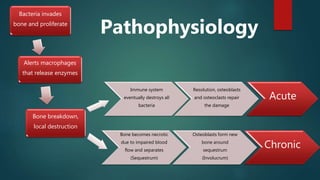
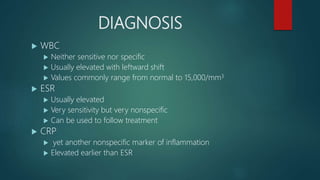
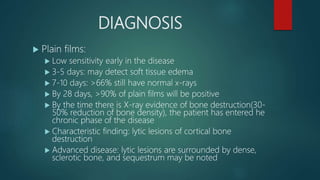
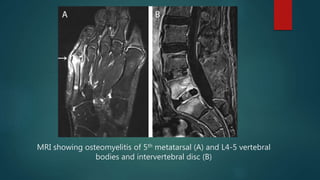
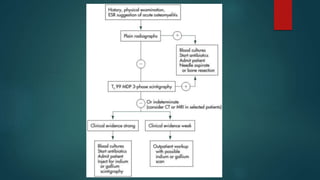
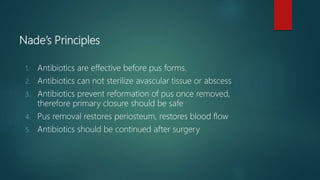
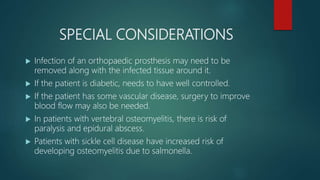
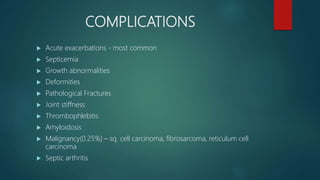
Osteomyelitis is an inflammation of the bone often caused by infection, manifesting in various forms depending on its cause, with common pathogens being Staphylococcus aureus. Risk factors include diabetes, immunosuppression, and surgical interventions, with symptoms ranging from bone pain to fever. Diagnosis may involve imaging and microbiologic tests, while treatment typically necessitates surgical debridement alongside antibiotic therapy for effective management.