This document provides information about scleral lens fitting, including:
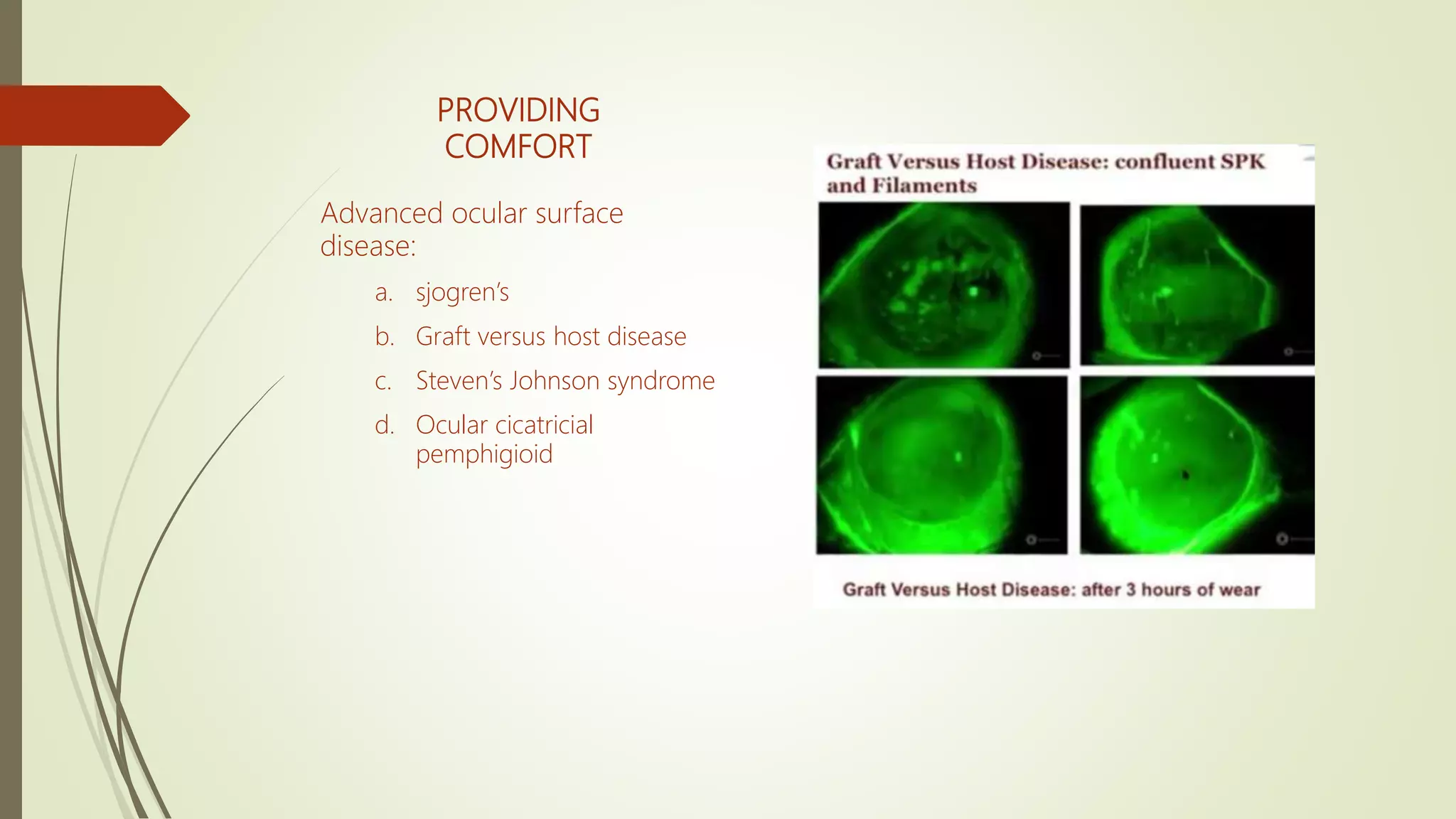
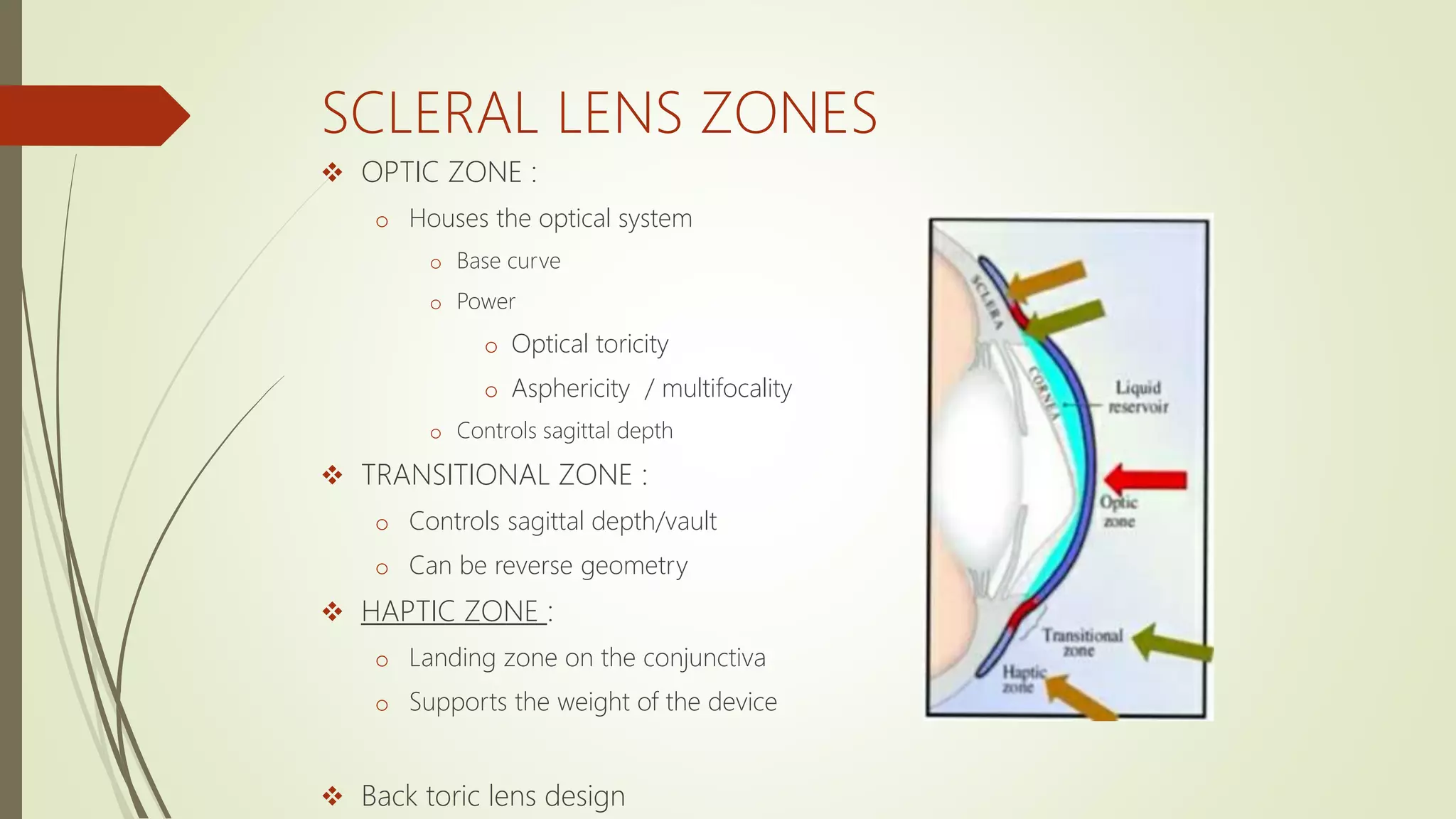
1) Scleral lenses are large diameter rigid contact lenses that cover the entire corneal surface and rest on the sclera, providing vision correction, protecting the ocular surface, and comfort.
2) Scleral lenses come in different types depending on their bearing area on the cornea and sclera, and are used to treat conditions like keratoconus as well as postoperative complications.
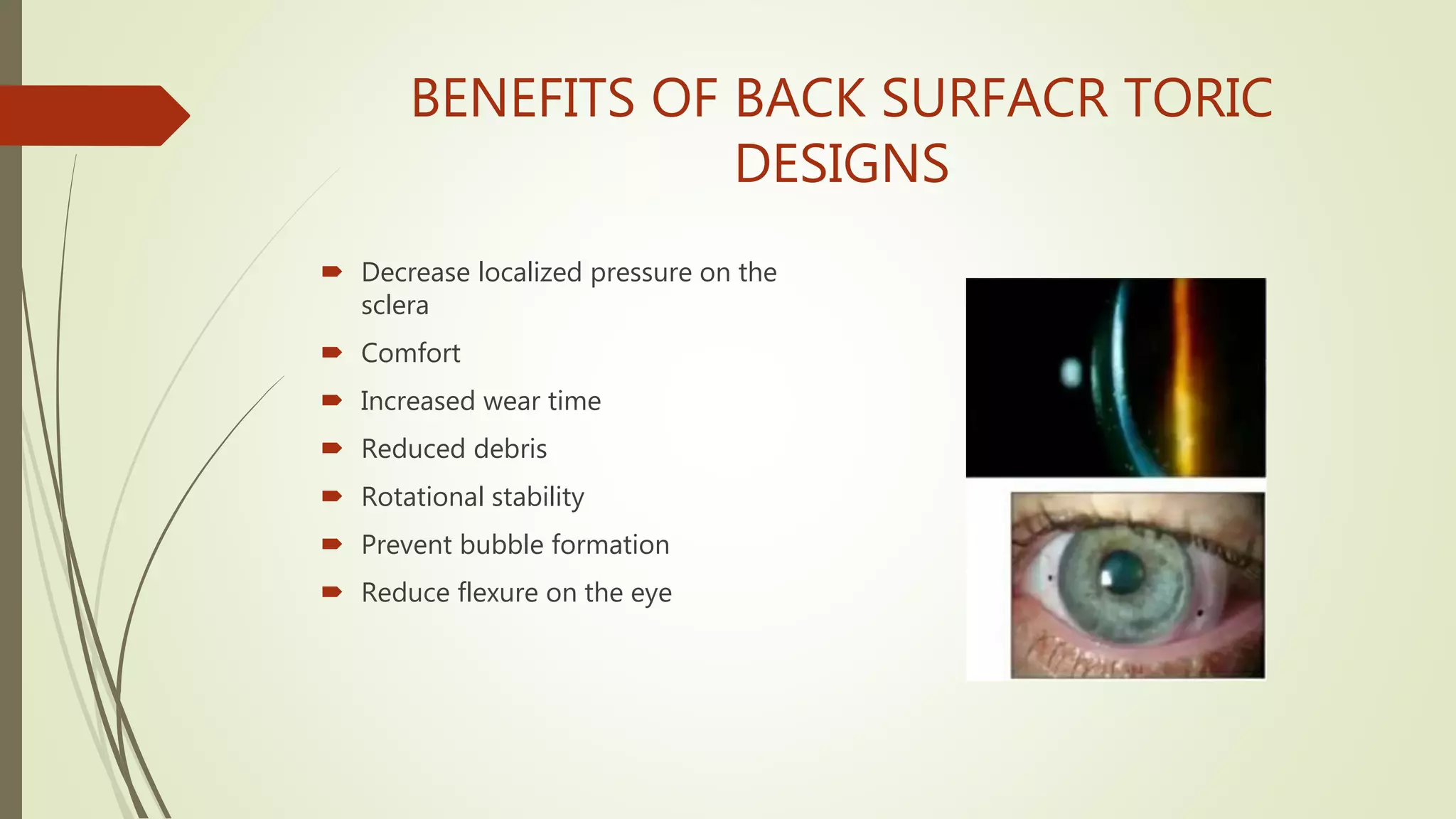
3) Fitting scleral lenses requires determining clearance, and can be time-consuming due to potential refits and frequent visits, but benefits include decreased pressure on the sclera and improved comfort and stability.