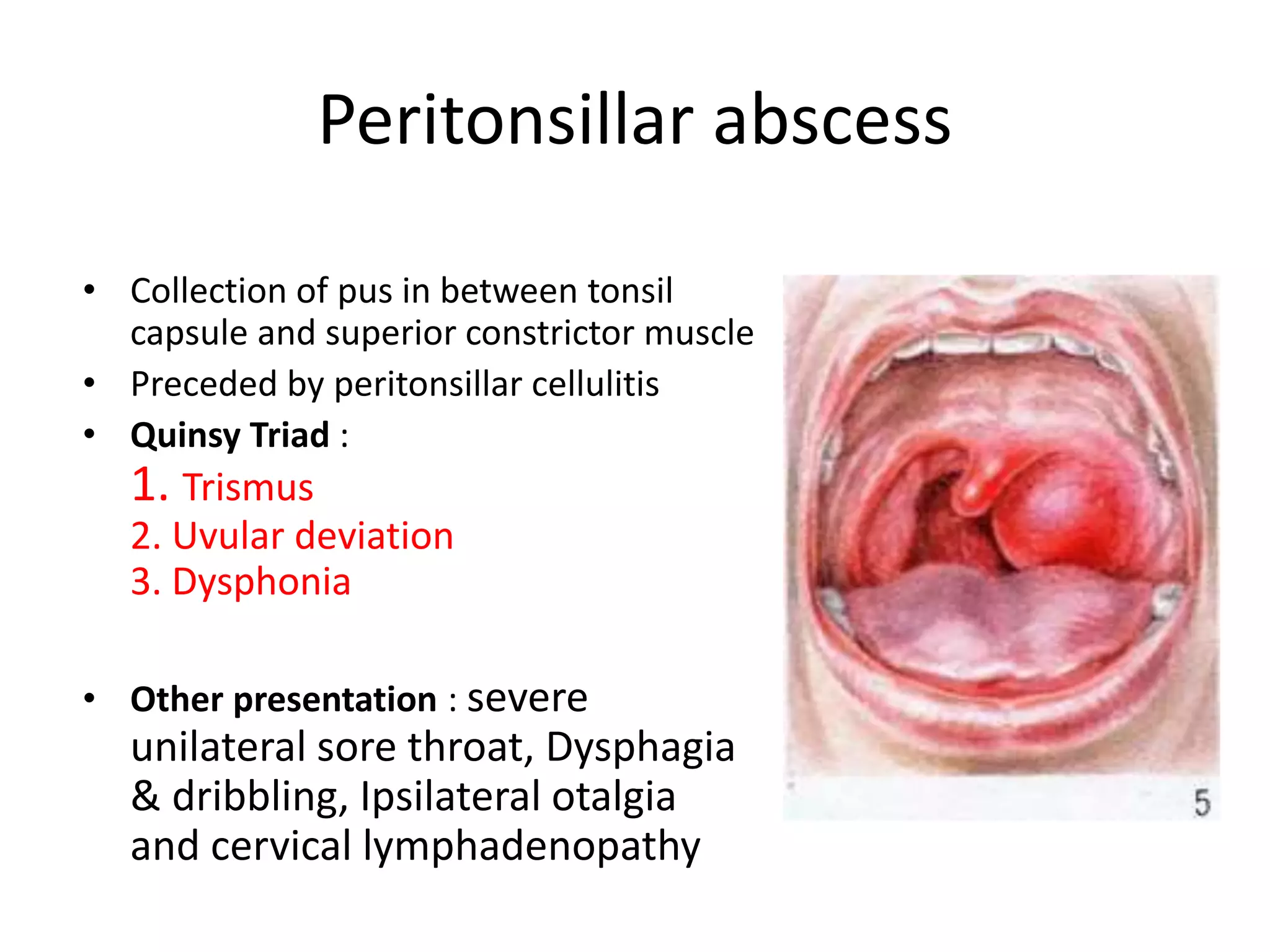
This document discusses various conditions that can cause sore throat, including common viral and bacterial infections as well as more serious conditions. It describes the symptoms, diagnosis, and treatment of several conditions in detail, such as tonsillitis, acute pharyngitis, peritonsillar abscess, and adenoid hypertrophy. Sore throat can be caused by streptococcal or other bacterial infections, viruses, or enlarged adenoids pressing on the throat. Accurate diagnosis and appropriate use of antibiotics or surgery are important for properly managing sore throat and preventing potential complications.