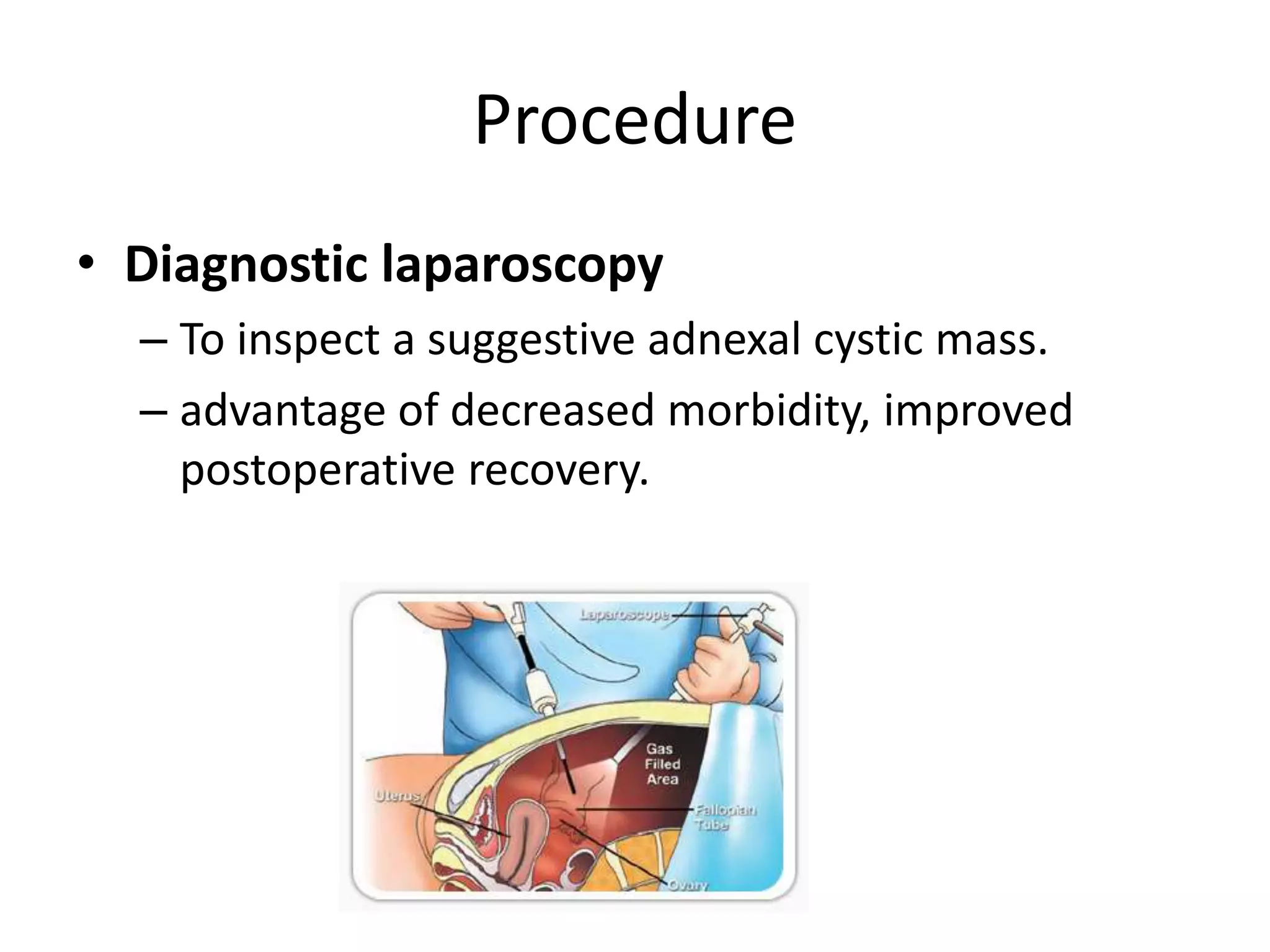
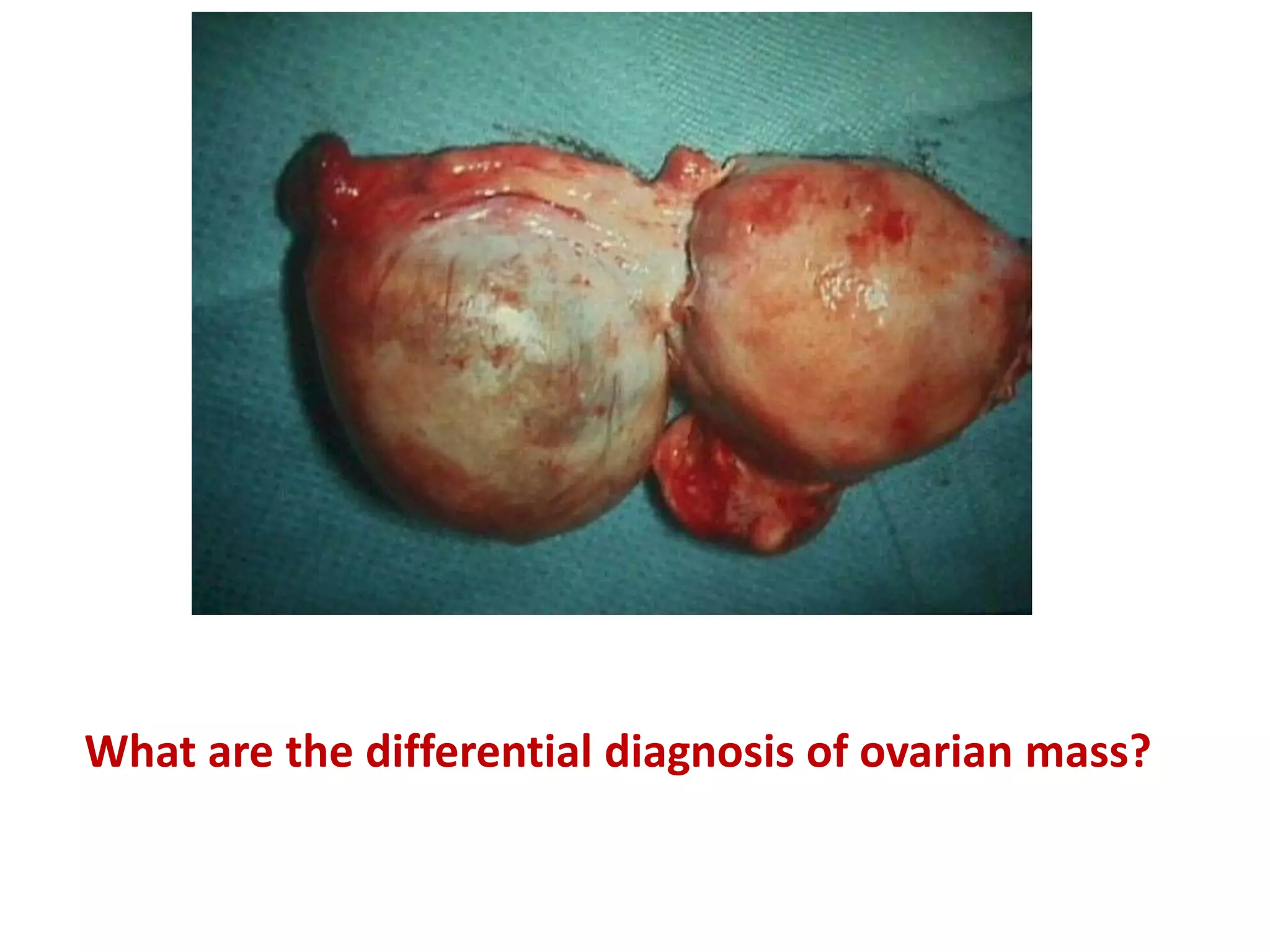
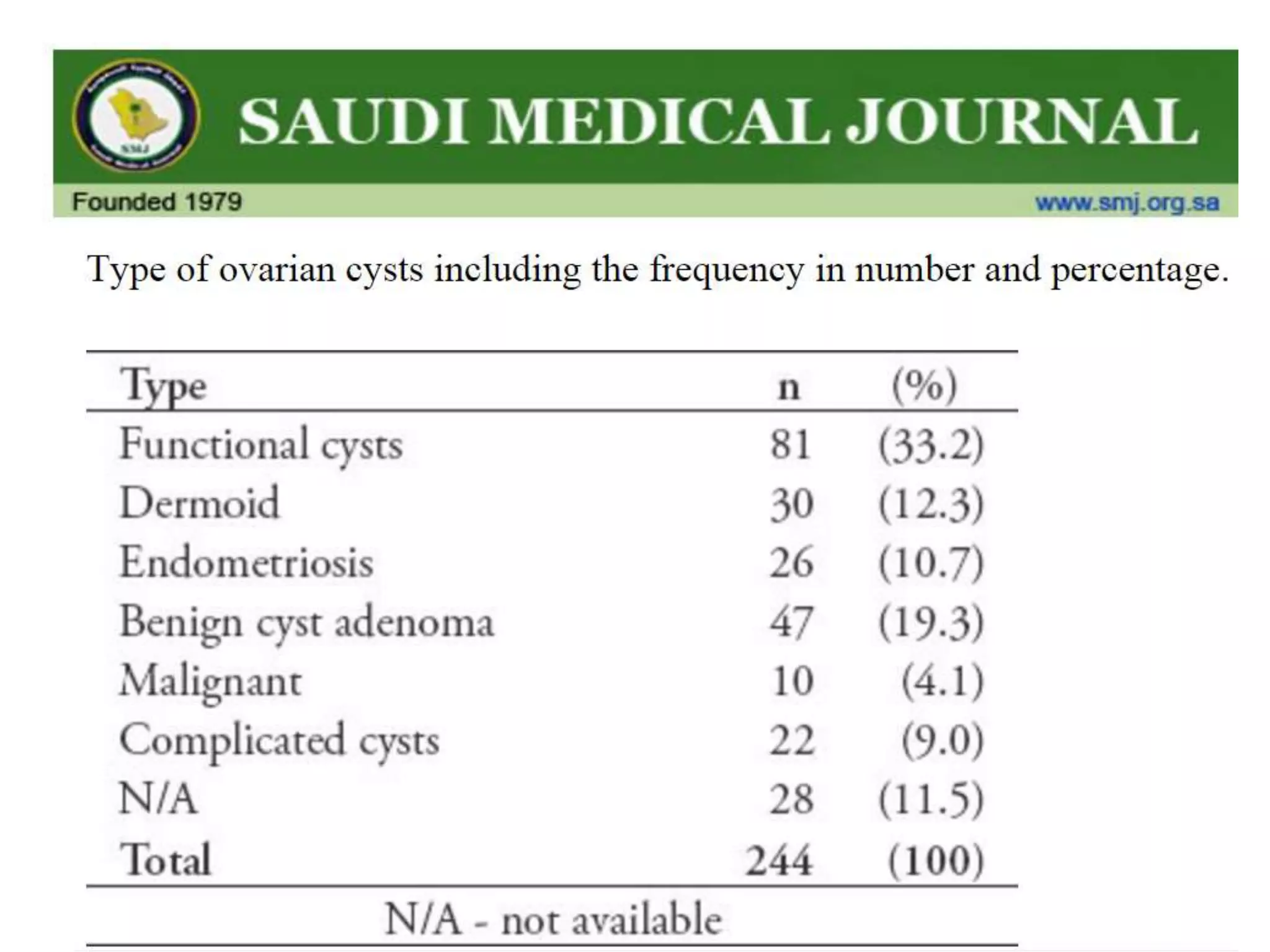
A 19-year-old woman presented with left lower abdominal pain and a history of ovarian cysts seen on prior imaging. On examination, she had tenderness in her lower abdomen. Ultrasound showed a new 5 cm hemorrhagic cyst on her left ovary. She underwent a laparoscopic cystectomy which found a hemorrhagic cyst with clots but no torsion. Her postoperative course was uncomplicated. Ovarian cysts are common and most are functional, resolving without treatment. Evaluation involves history, exam, ultrasound and considering tumor markers or laparoscopy if concerned for a neoplasm.