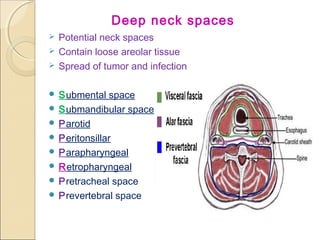
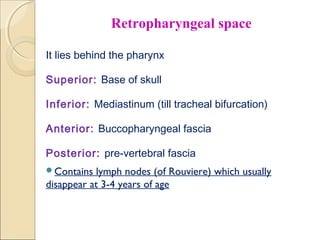
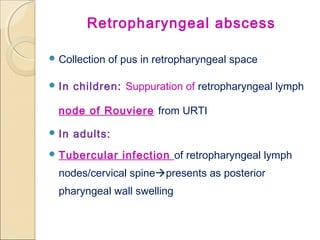
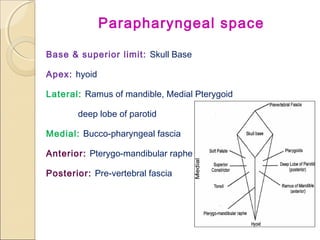
1. The document discusses various deep neck spaces and infections that can arise within them, including Ludwig's angina (submandibular space infection), retropharyngeal abscess, and parapharyngeal abscess.
2. These deep neck space infections commonly arise from dental infections or tonsillitis and can spread rapidly, potentially causing airway obstruction.
3. Management involves intravenous antibiotics, incision and drainage of abscesses, and tracheostomy if needed to secure the airway. Proper identification of the involved neck space guides surgical drainage approach.