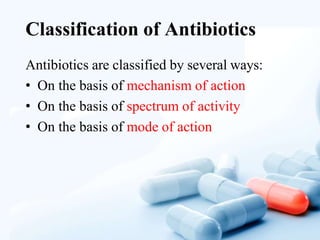
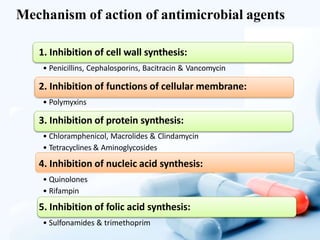
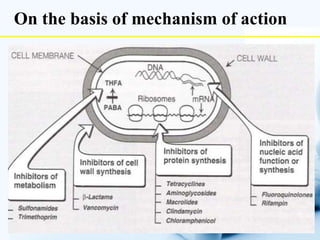
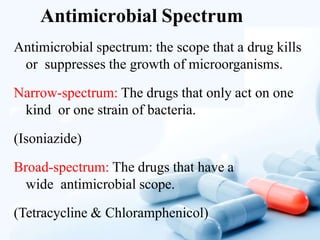
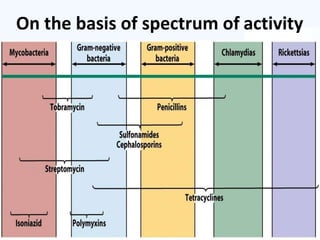
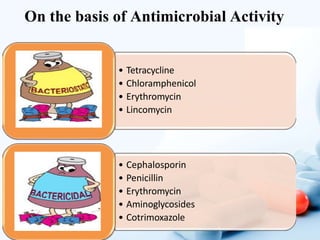
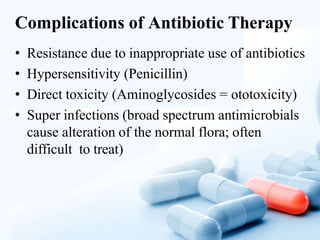
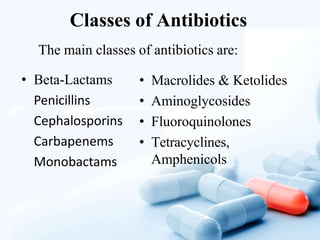
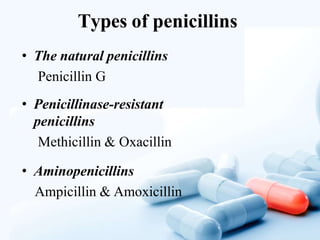
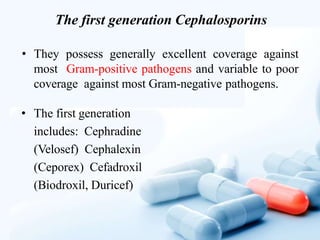
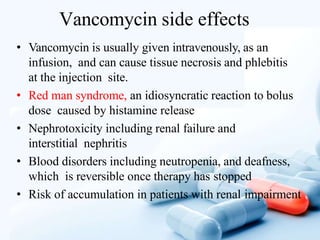
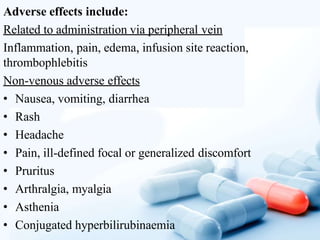
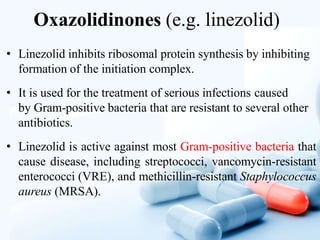
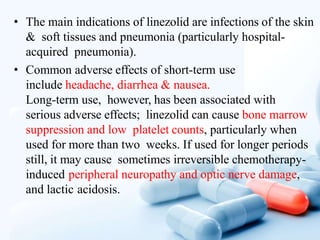
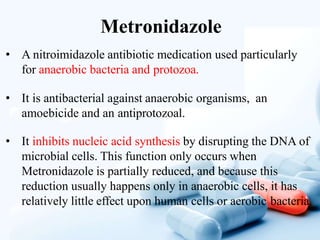
This document provides an overview of different classes of antibiotics, including their mechanisms of action, uses, and side effects. It discusses beta-lactam antibiotics like penicillins and cephalosporins, as well as macrolides, fluoroquinolones, aminoglycosides, tetracyclines, chloramphenicol, glycopeptides and others. Each class is described in terms of its antimicrobial spectrum and applications for treating various bacterial infections. Potential adverse effects are also outlined for safety considerations.