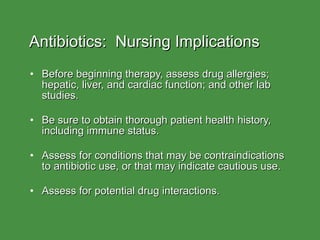
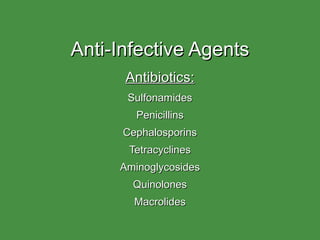
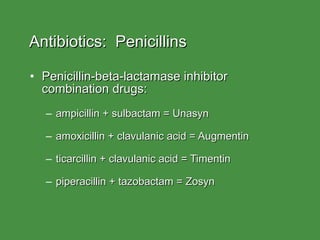
The document discusses various classes of anti-infective agents (antibiotics), including their mechanisms of action, therapeutic uses, and common side effects. It covers sulfonamides, penicillins, cephalosporins, tetracyclines, aminoglycosides, quinolones, and macrolides. For each class, it provides one to three examples of commonly used drugs and briefly outlines their antimicrobial spectrum, dosing routes, and adverse effect profiles.








































![Aminoglycosides Three most common (systemic): gentamicin, tobramycin, amikacin Cause serious toxicities: Nephrotoxicity (renal failure) Ototoxicity (auditory impairment and vestibular [eighth cranial nerve]) Must monitor drug levels to prevent toxicities](https://image.slidesharecdn.com/antibiotics-100421001252-phpapp01/85/Antibiotics-43-320.jpg)