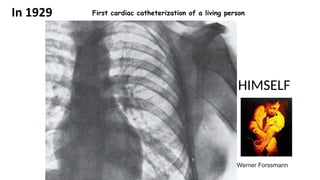
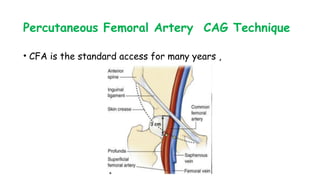
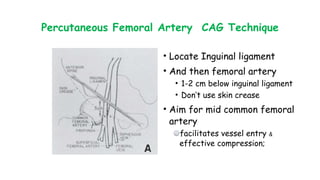
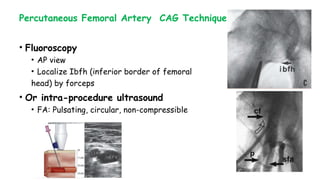
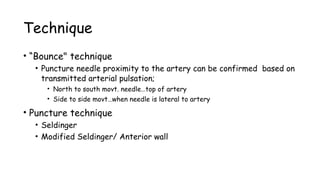
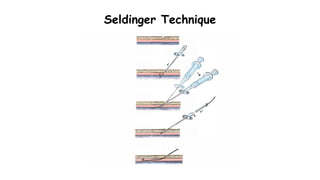
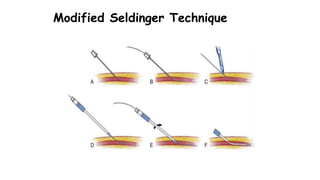
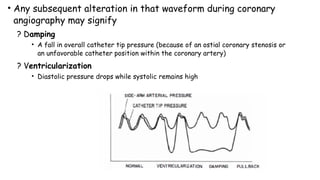
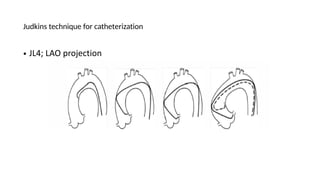
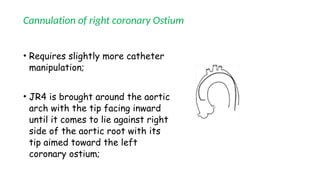
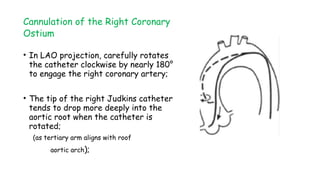
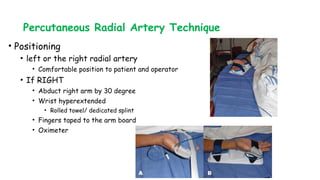
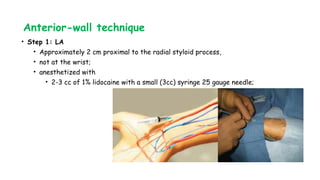
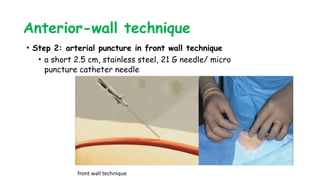
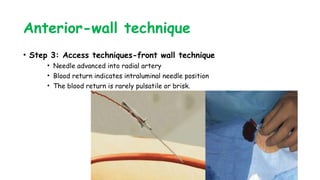
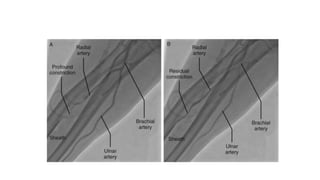
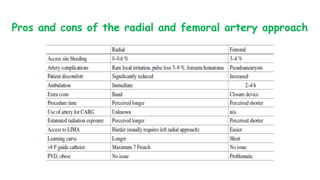
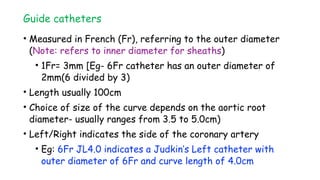
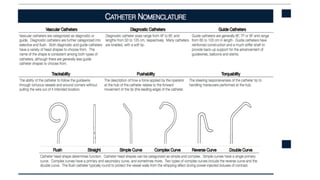
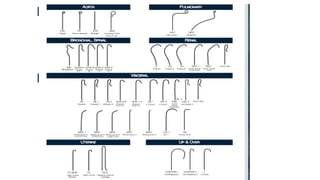
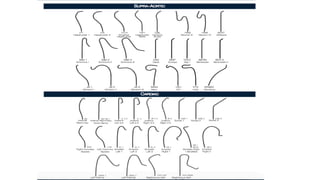
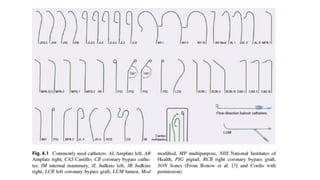
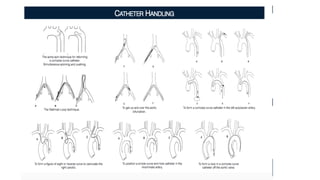
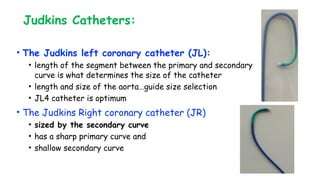
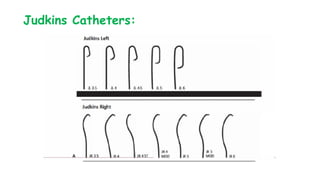
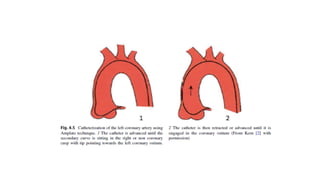
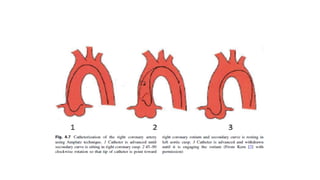
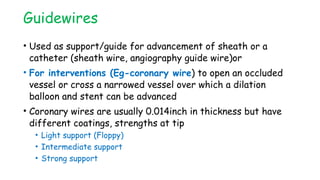
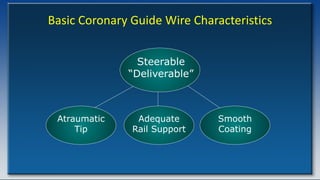
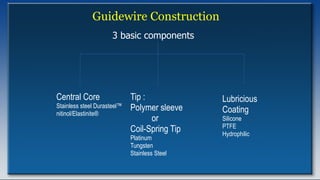
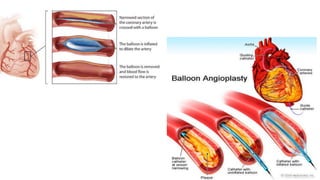
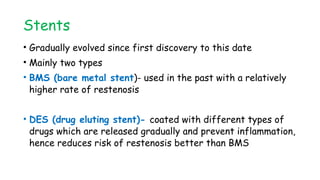
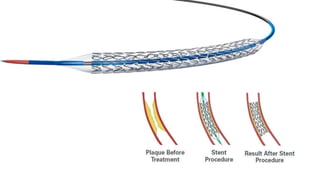
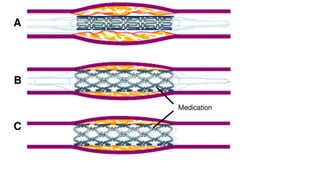
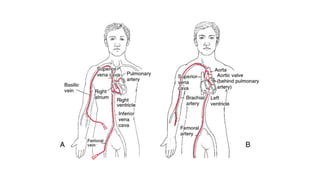
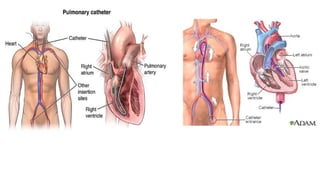
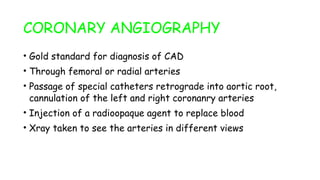
This document provides a brief history and overview of common devices and procedures used in interventional cardiology. It discusses the development of cardiac catheterization from early experiments in animals in the 18th century to modern percutaneous techniques. Key events included the first human cardiac catheterization in 1929 and the first percutaneous coronary angioplasty in 1977. The document then describes techniques for vascular access, coronary cannulation, and performing coronary angiography and angioplasty procedures via the femoral or radial arteries.