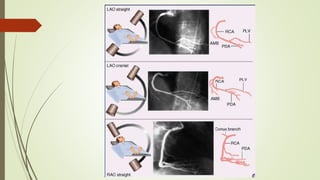
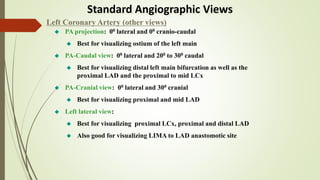
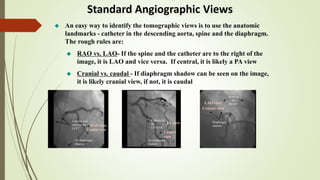
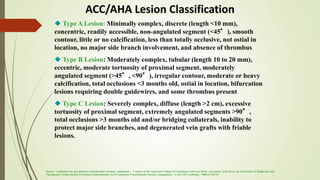
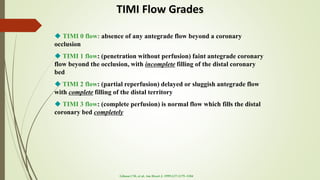
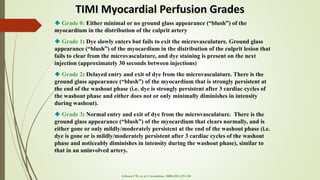
This document provides guidance on performing and interpreting coronary angiograms. It discusses techniques such as catheter selection, standard angiographic views, contrast injection settings, and complications. It also covers evaluating angiograms by quantifying lesions, classifying them using ACC/AHA criteria, and assessing TIMI flow. Interpretation involves a systematic analysis of the coronary anatomy and any areas of stenosis.