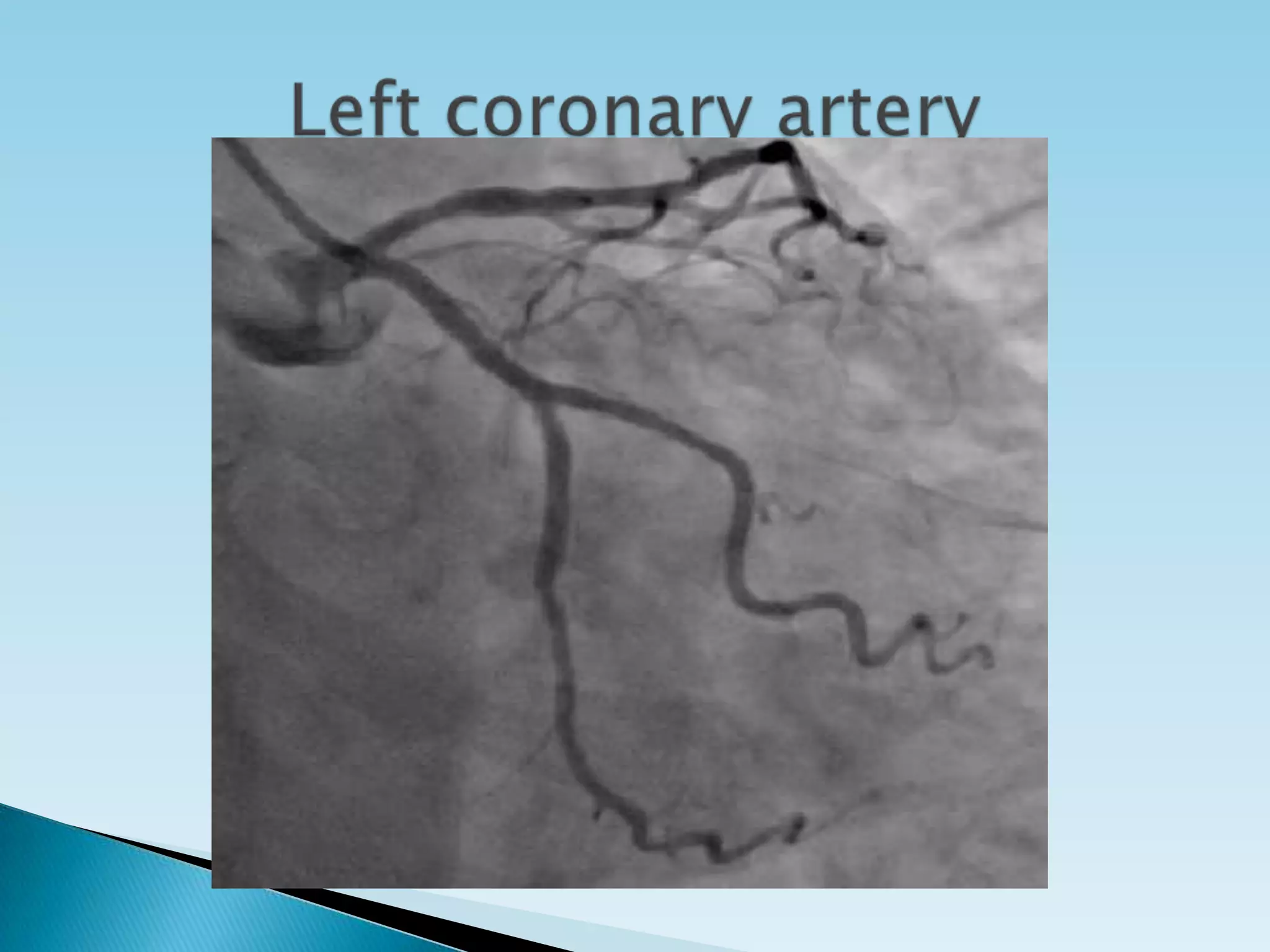
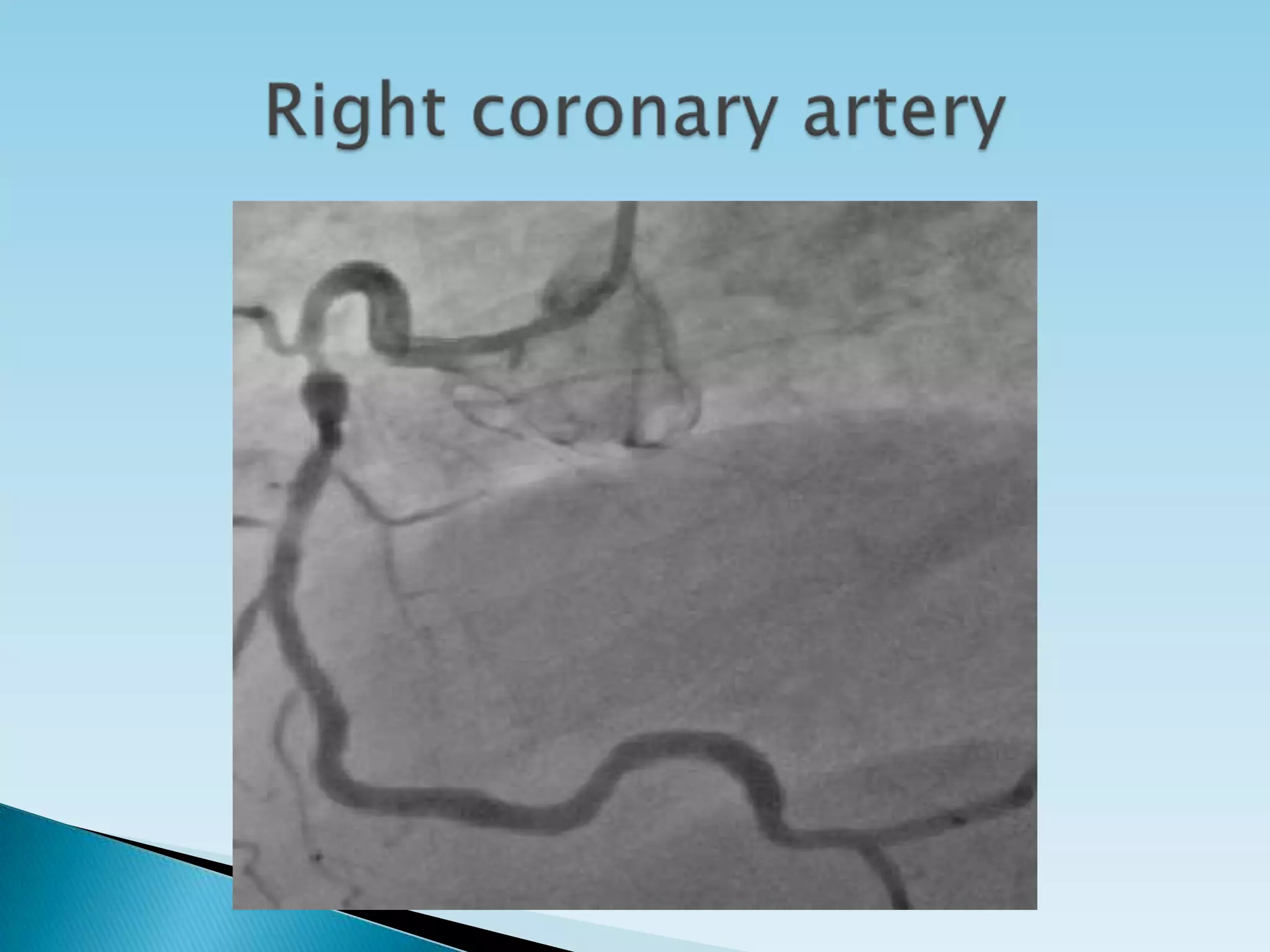
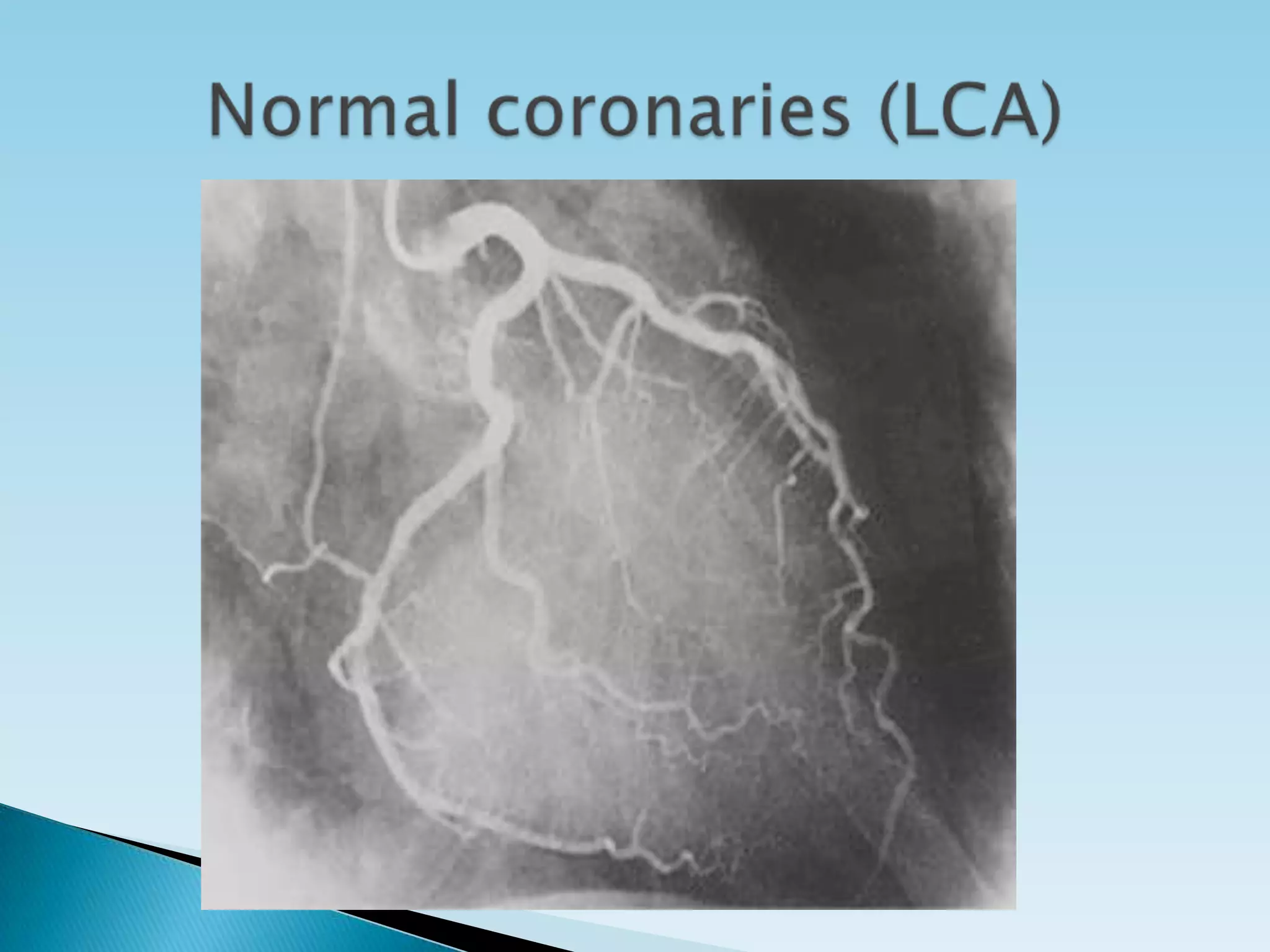
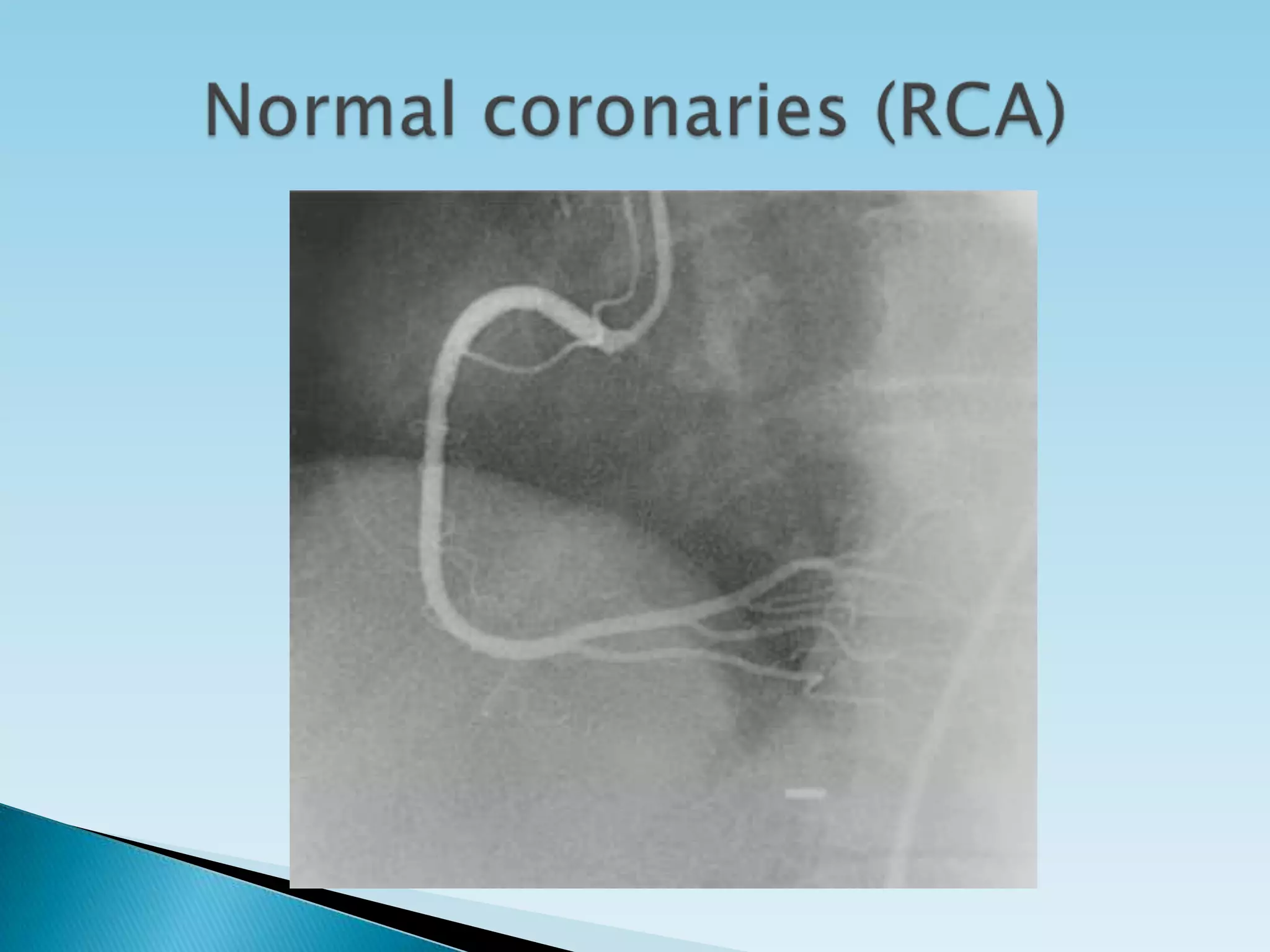
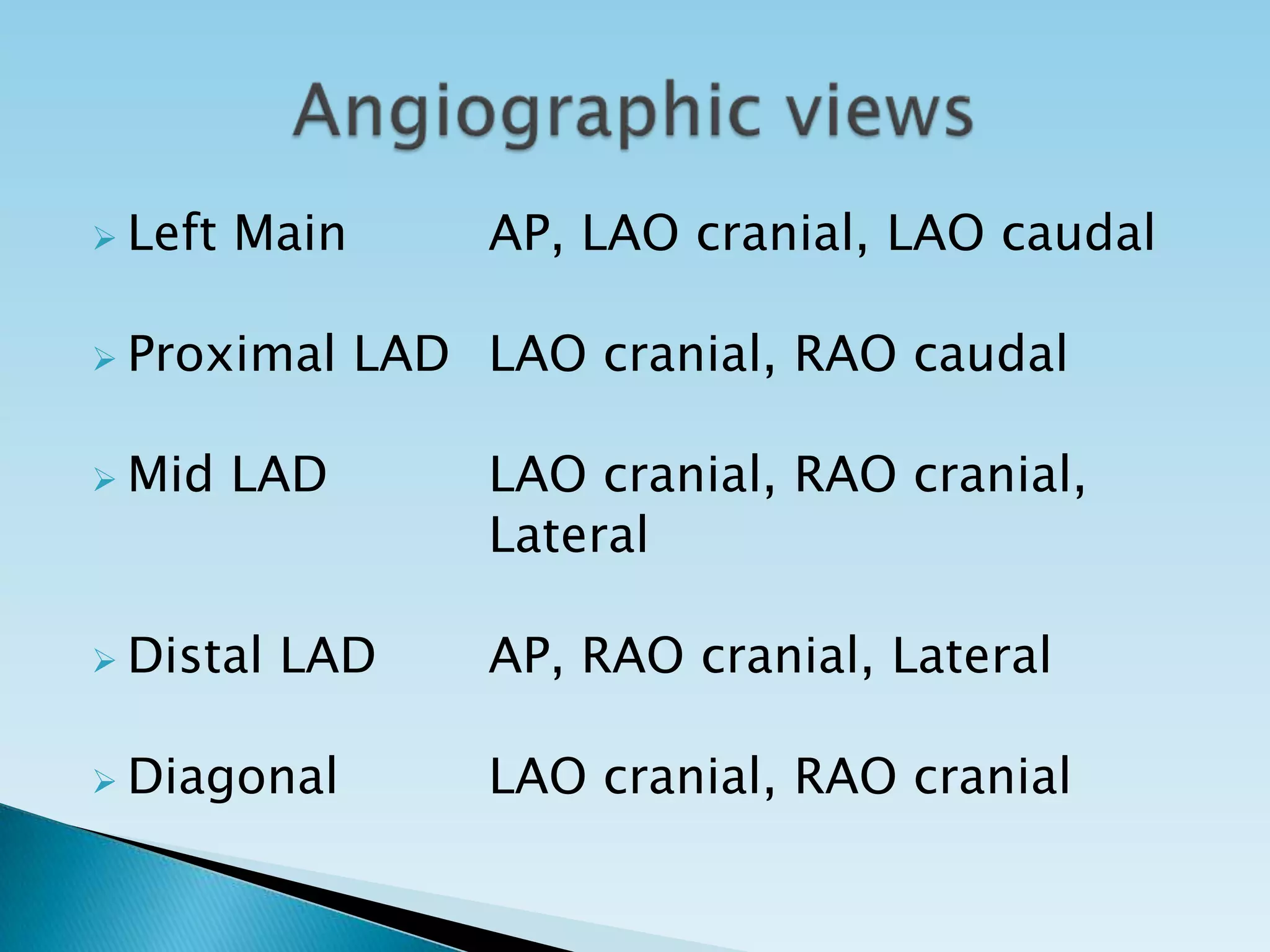
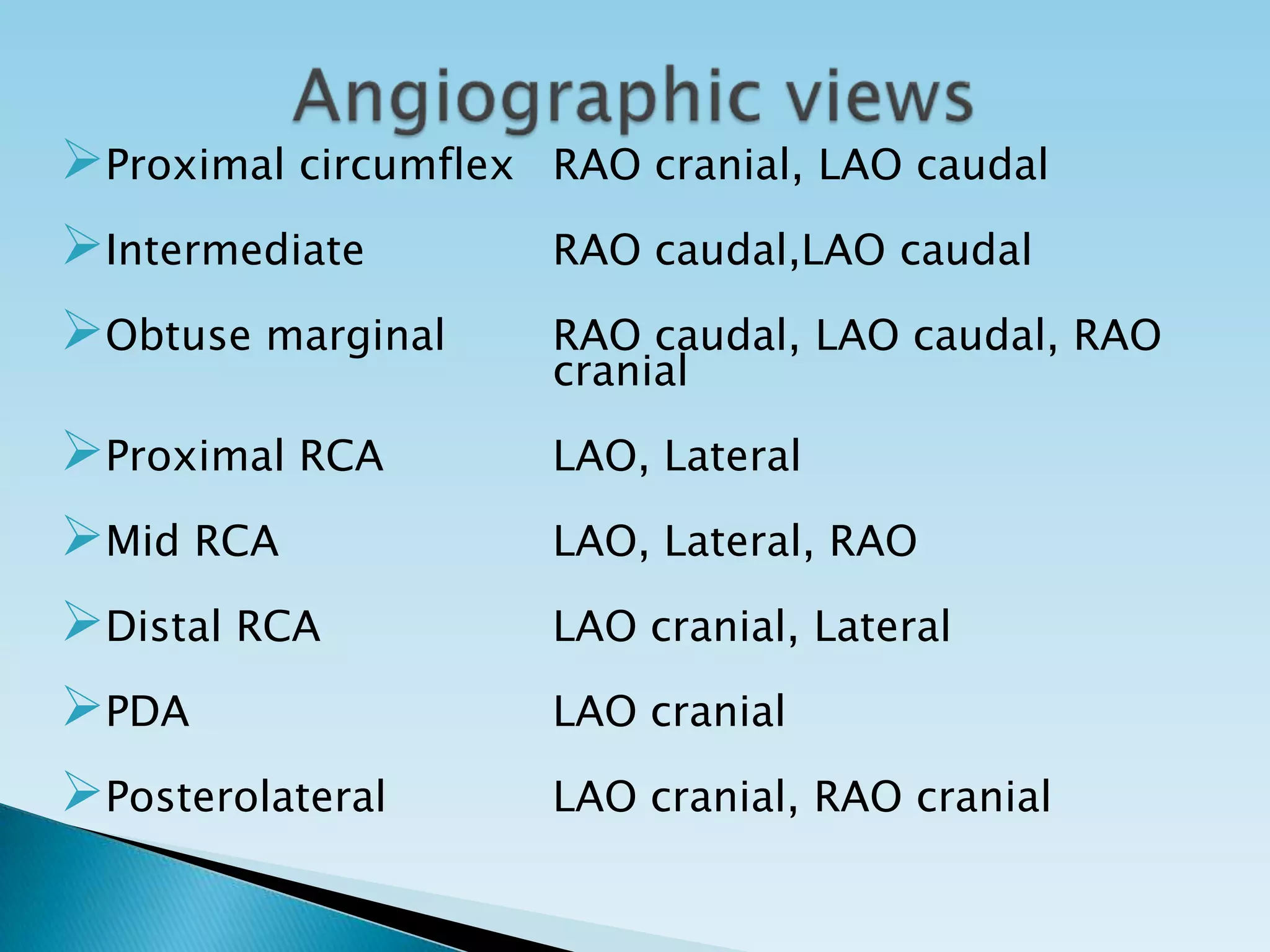
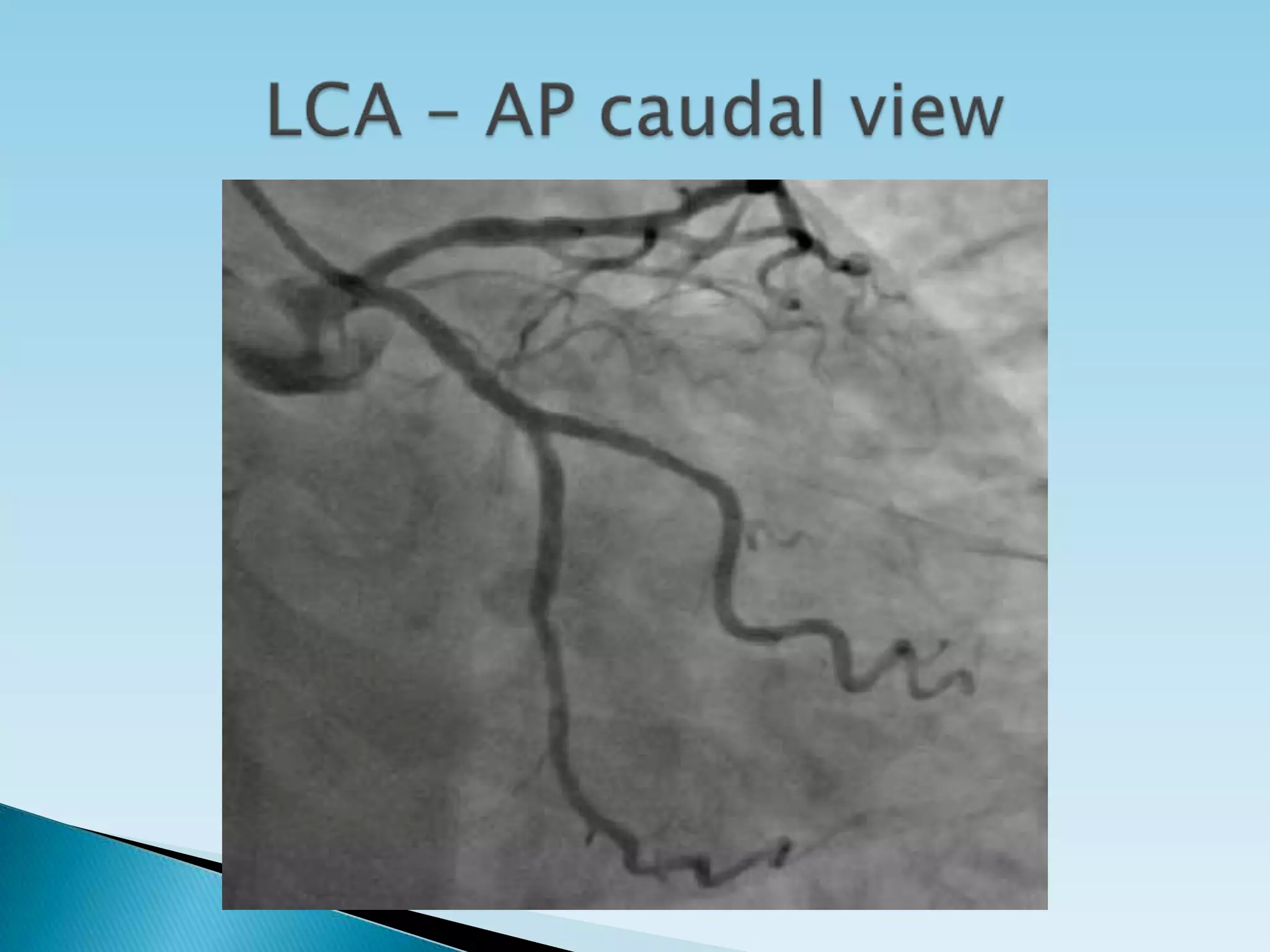
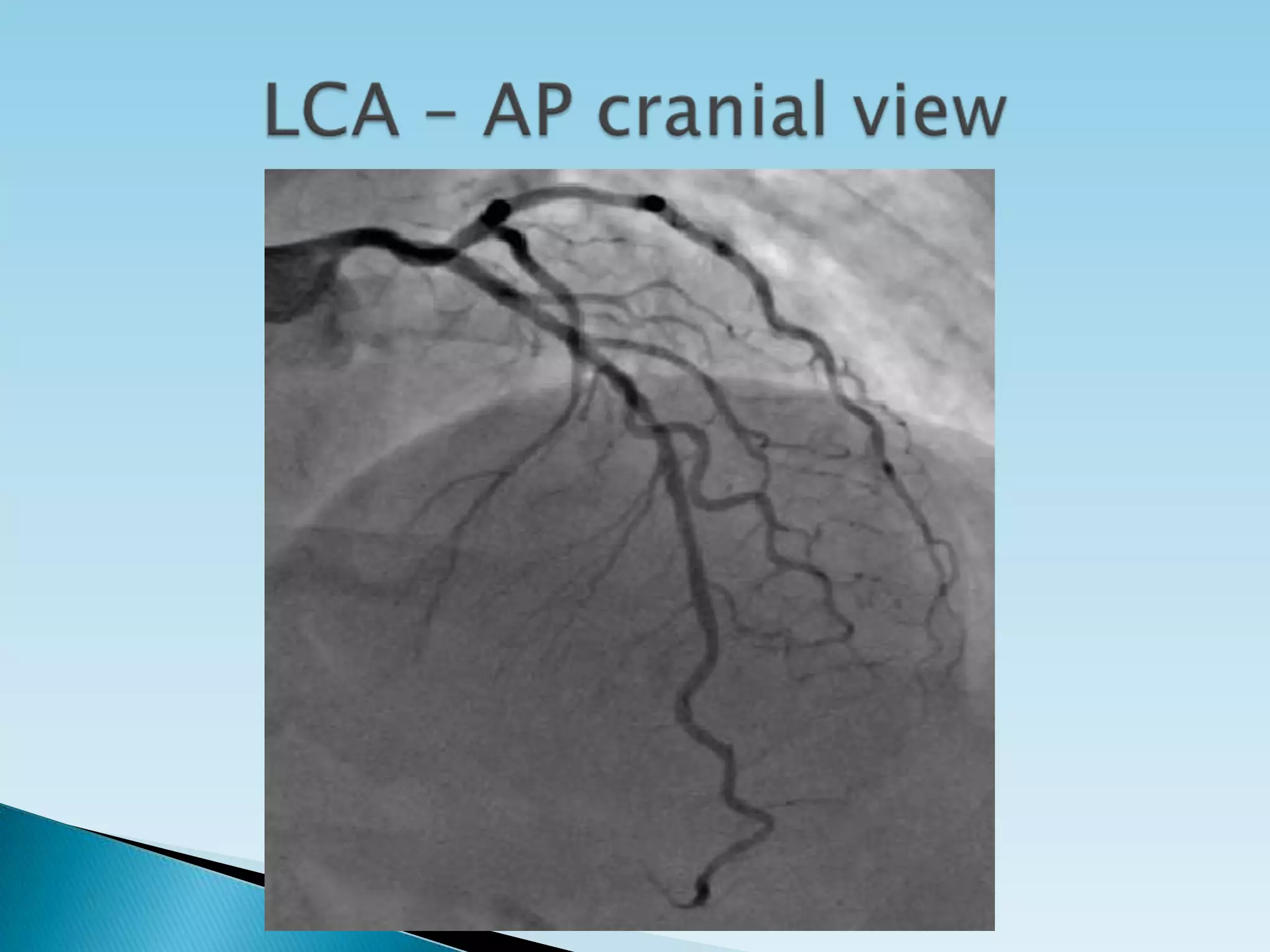
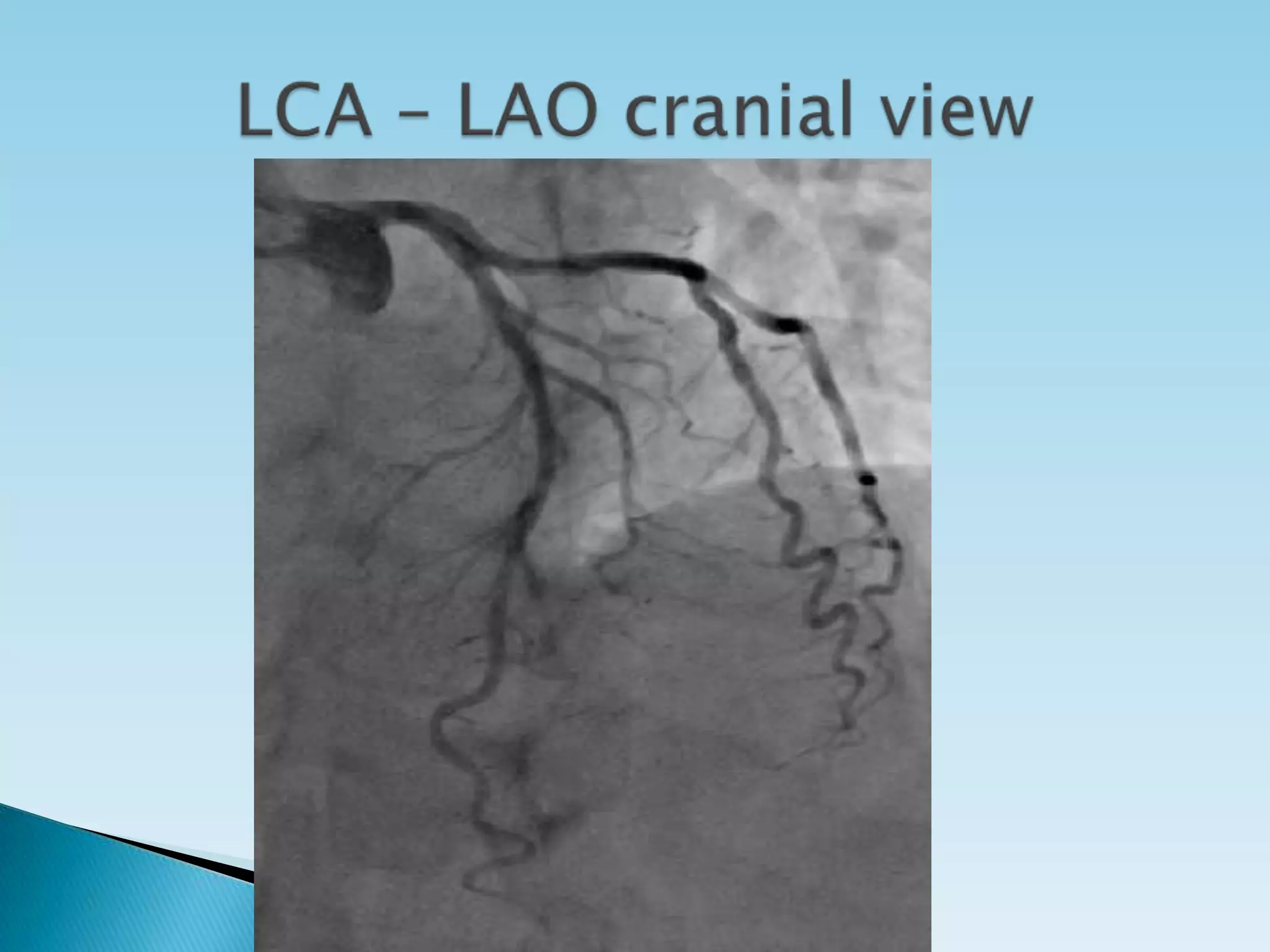
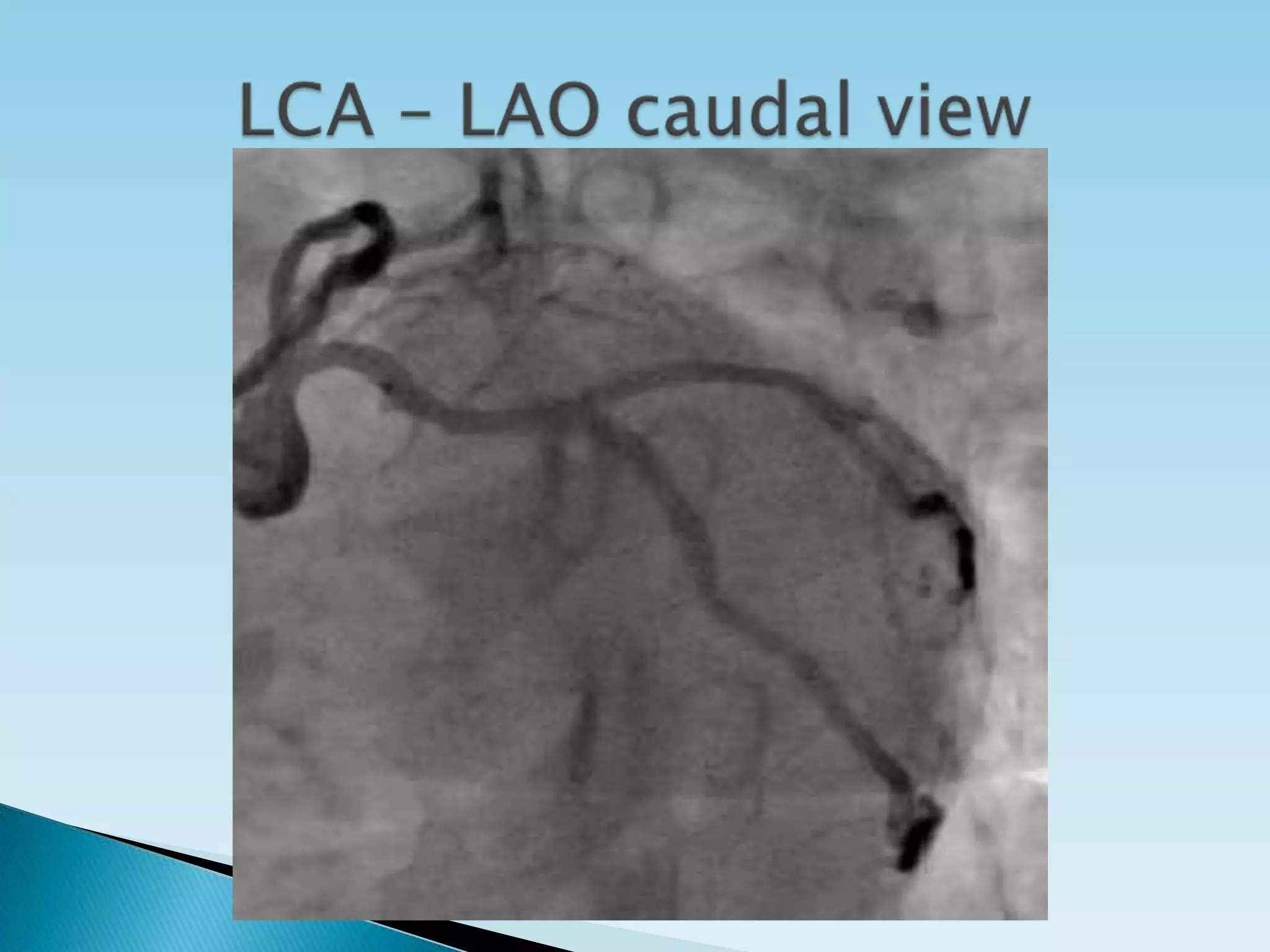
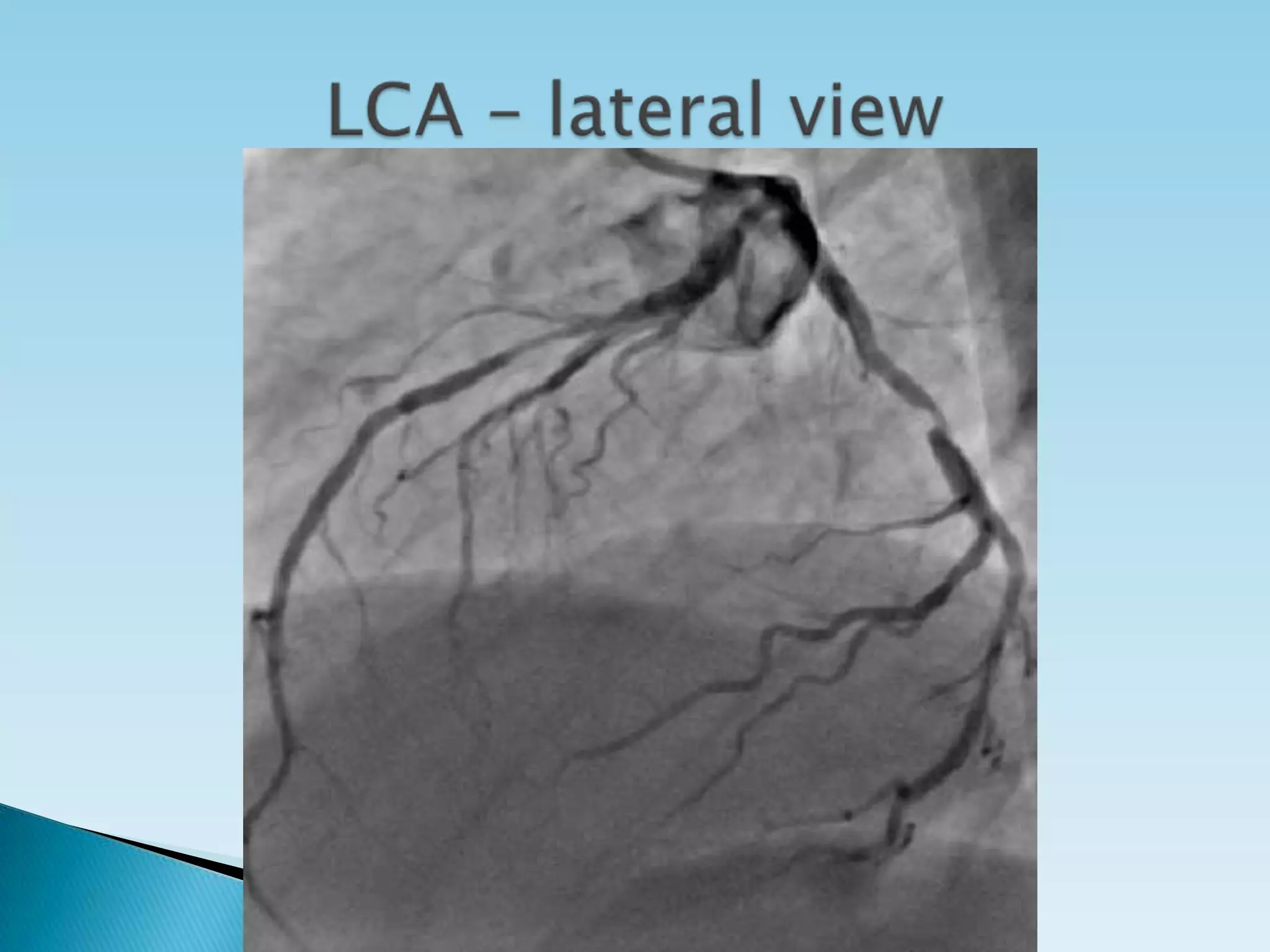
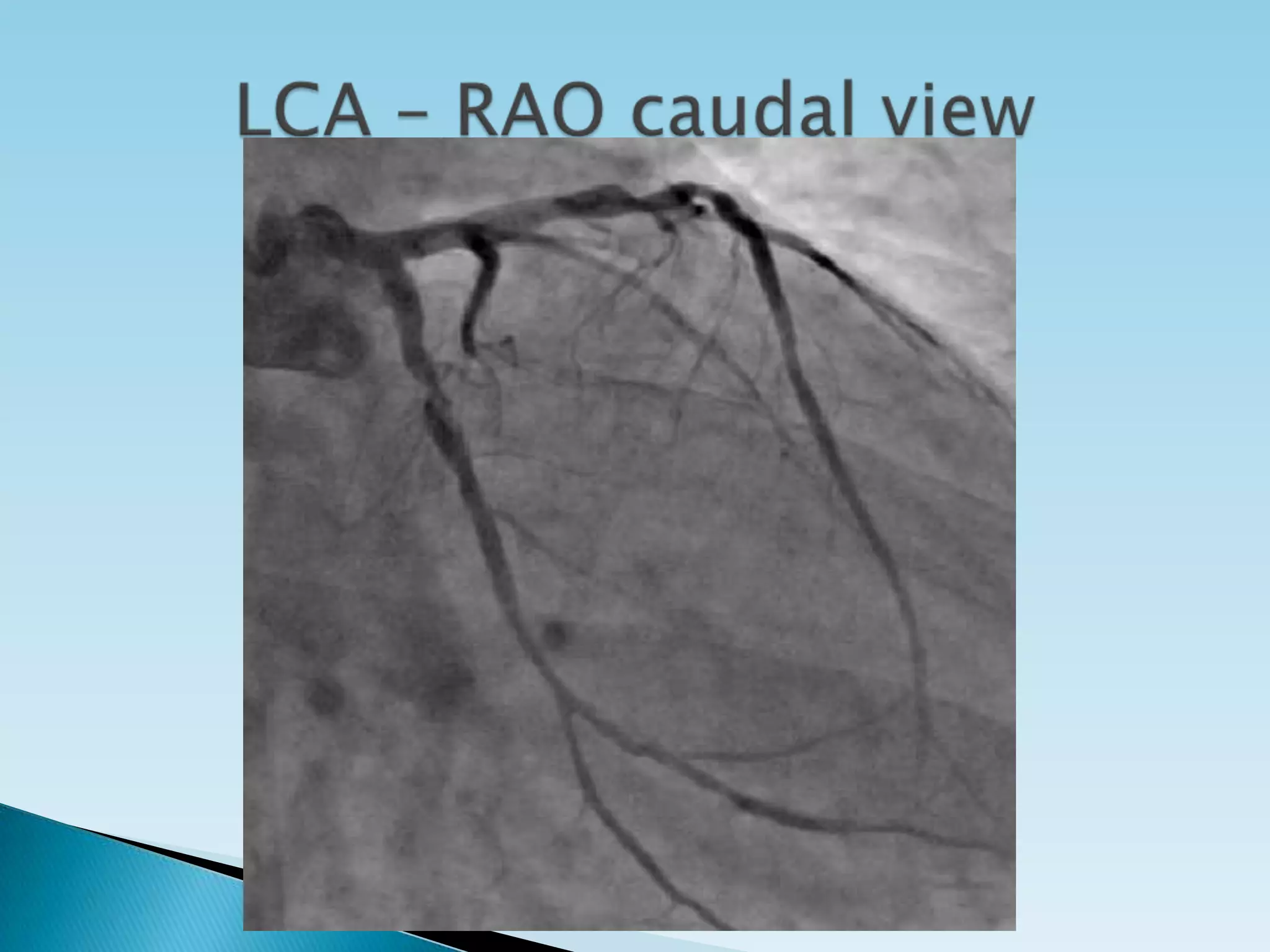
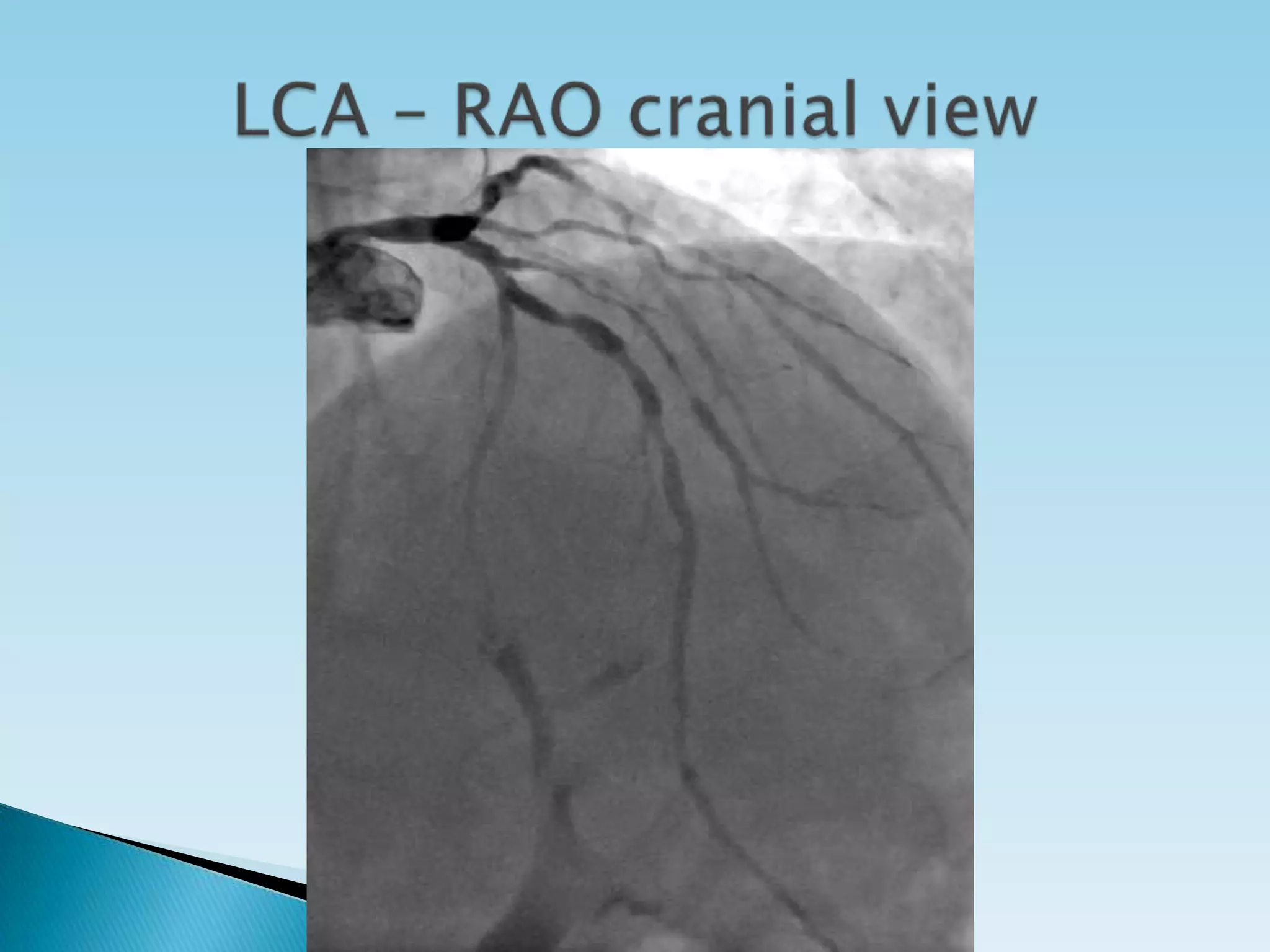
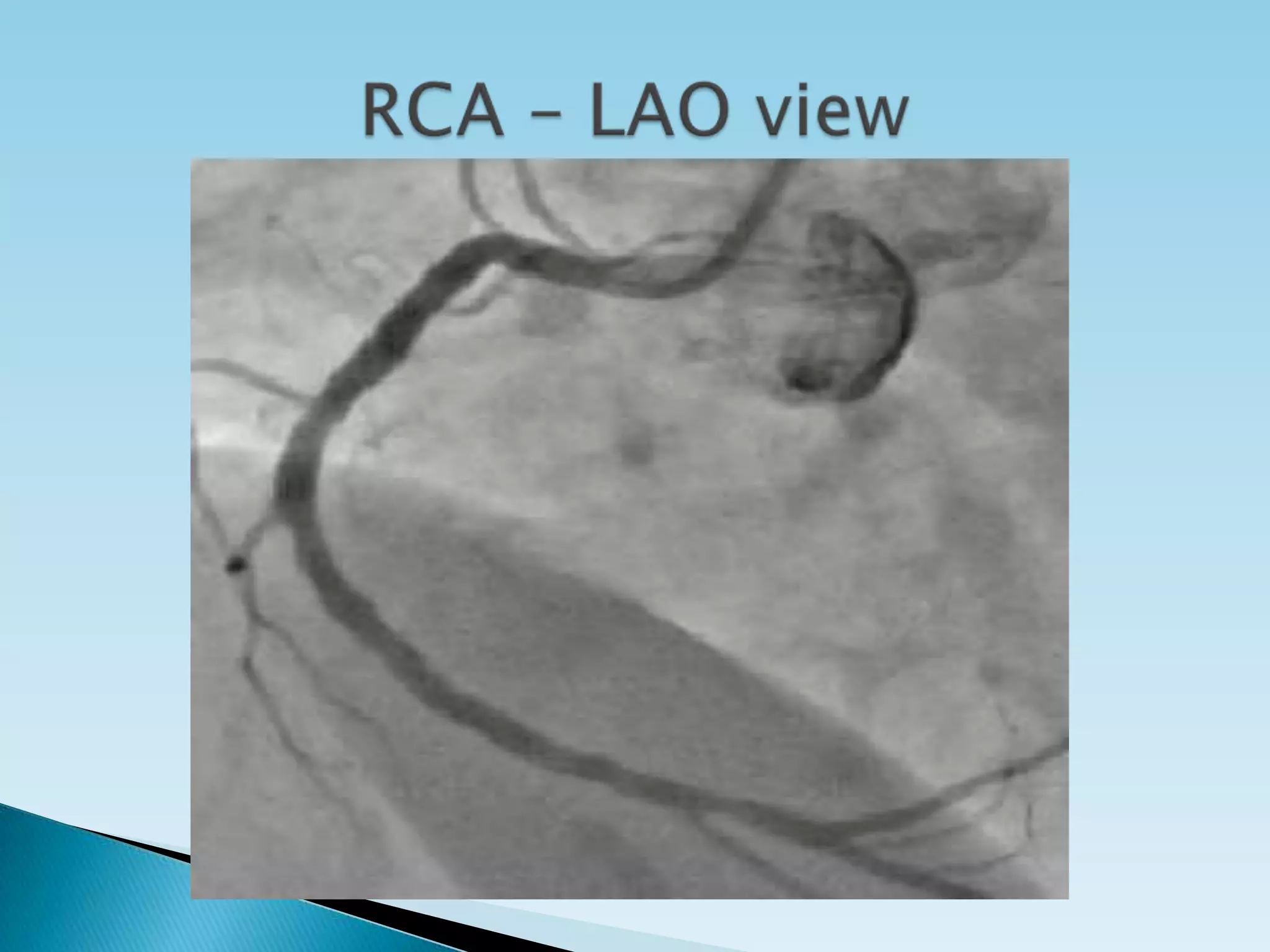
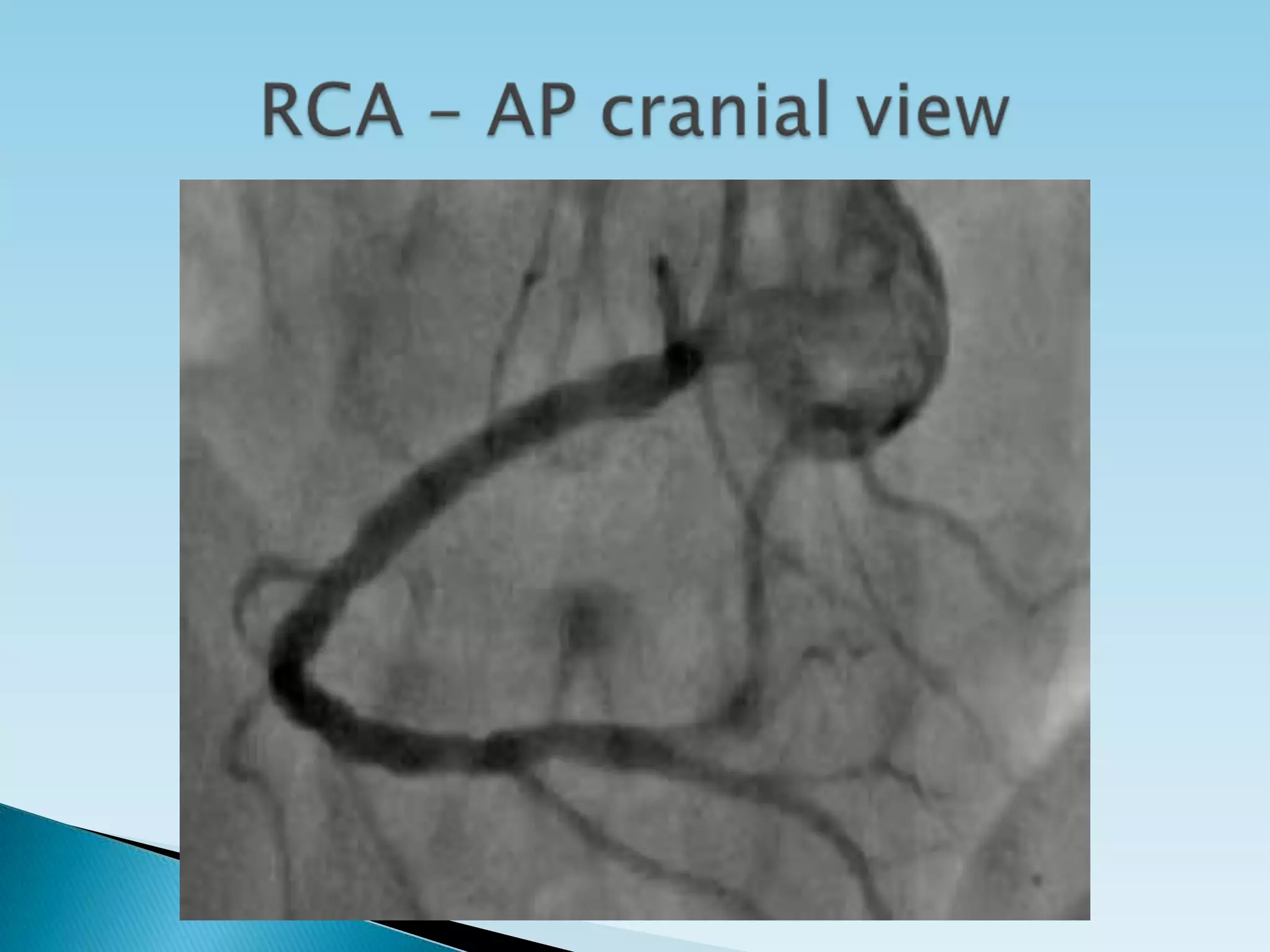
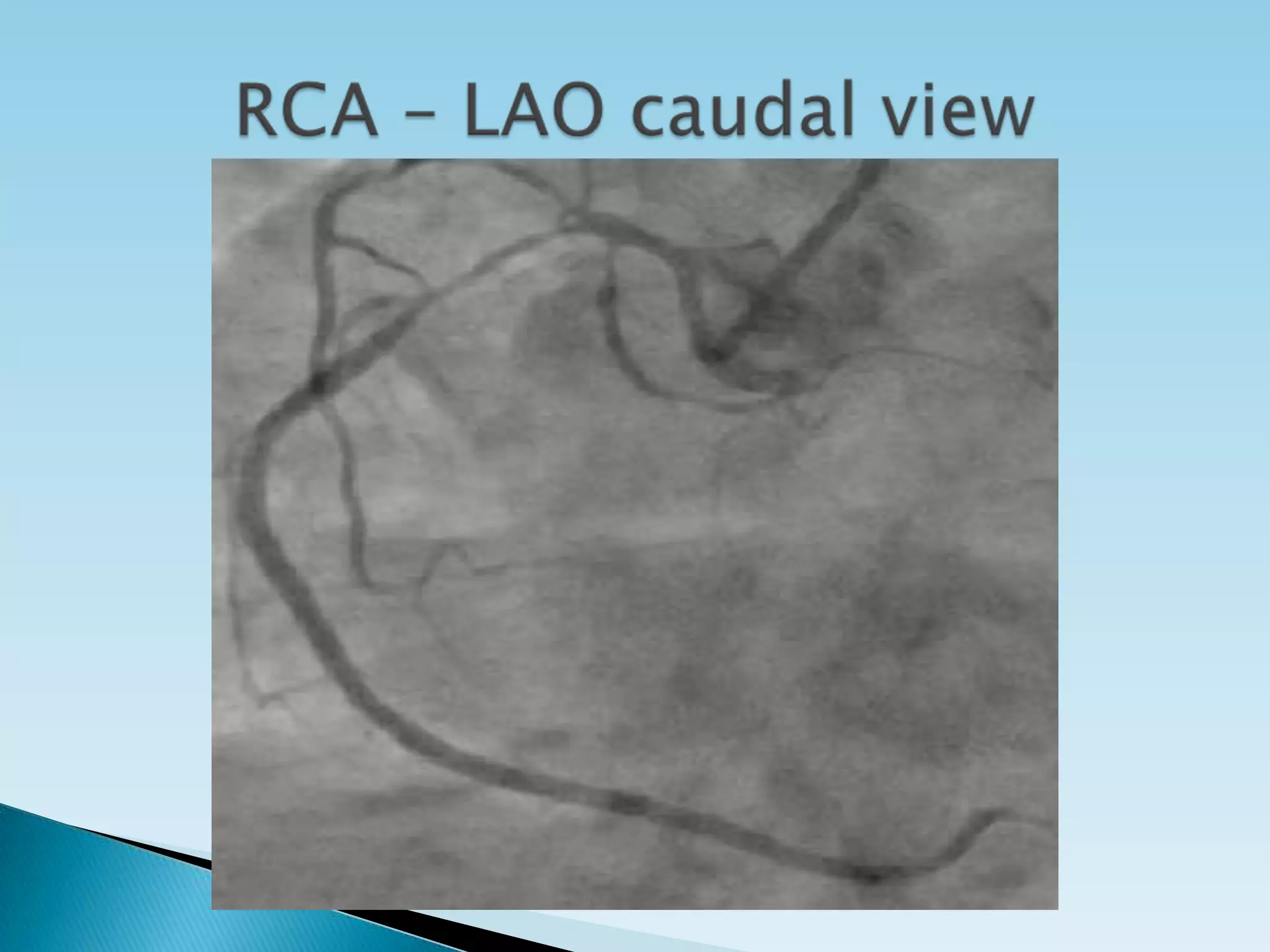
Coronary angiography remains the gold standard for detecting coronary artery disease. The technique was first performed in 1958 and is used to visualize the coronary arteries and assess for stenosis. It can determine treatment options and prognosis. Complications are rare but include vascular injury and contrast reactions. Proper angiographic views are important for evaluating different coronary artery segments.