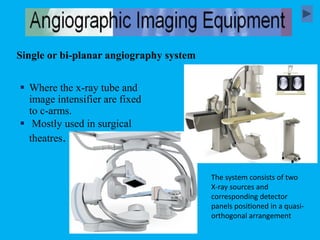
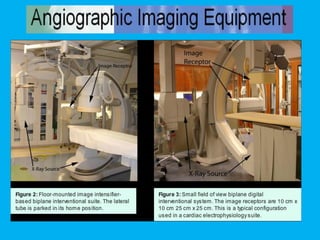
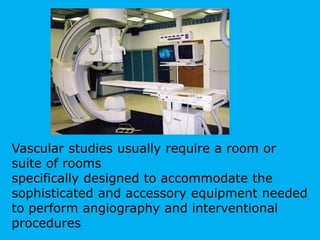
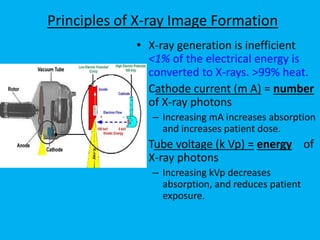
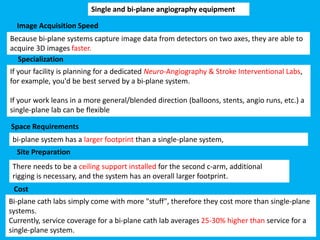
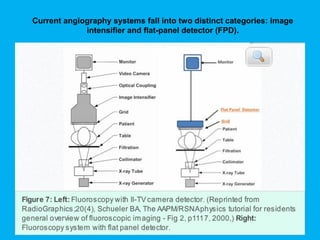
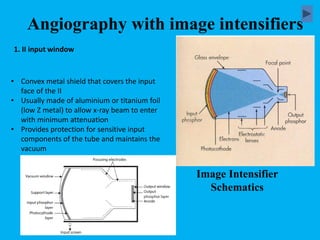
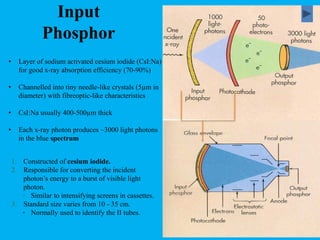
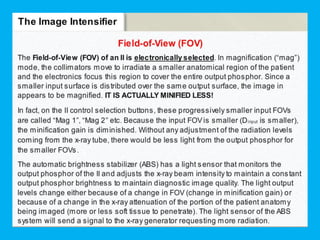
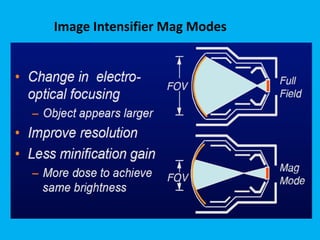
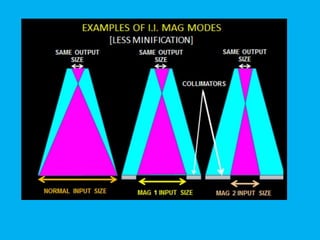
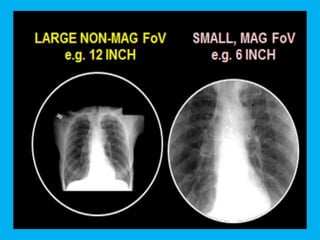
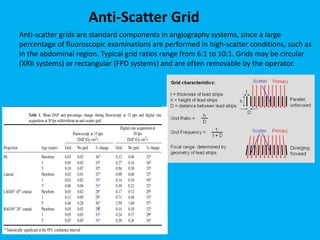
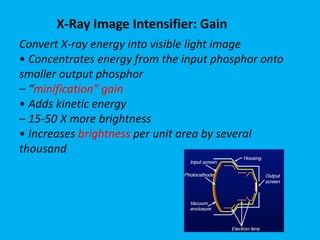
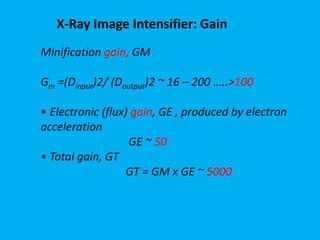
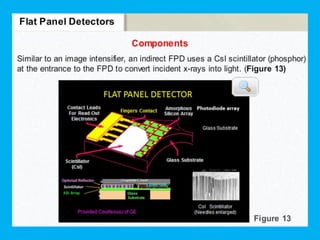
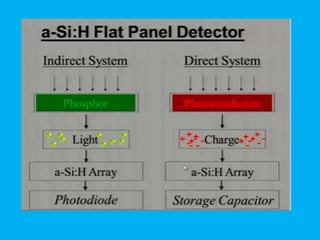
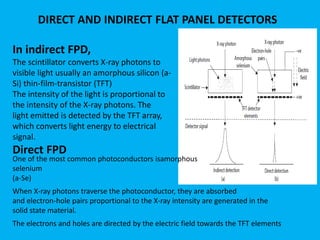
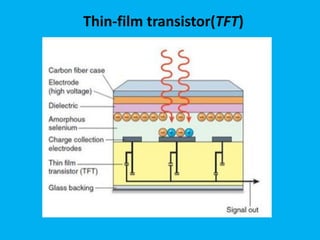
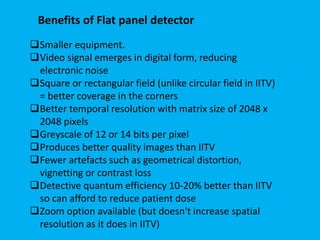
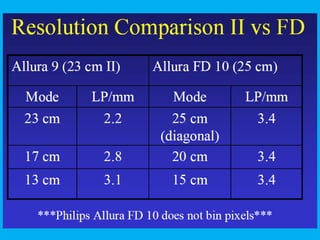
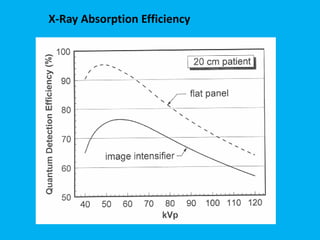
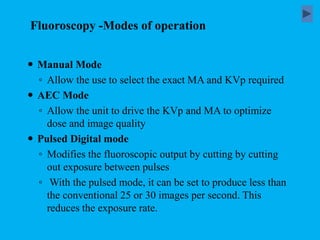
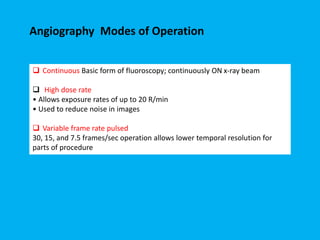
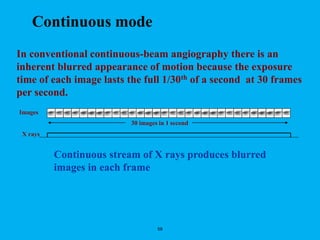
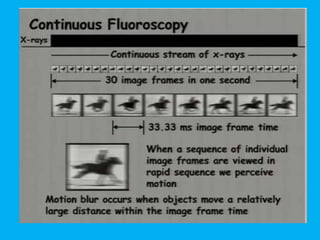
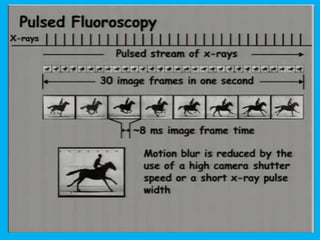
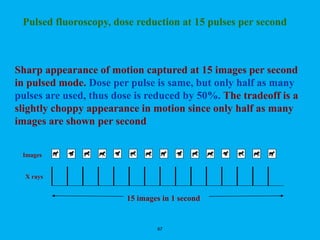
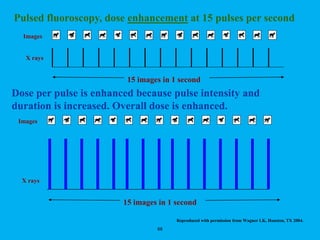
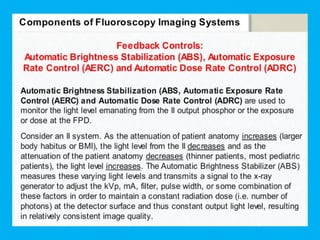
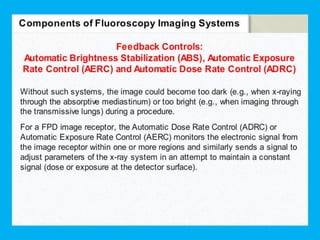
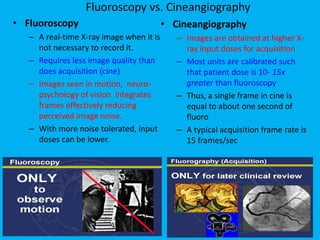
Angiography uses iodinated contrast medium and x-rays to visualize blood vessels. The document discusses the basic components of angiography equipment, including the x-ray tube, generator, patient table, beam filtration, collimation, anti-scatter grid, and image receptor. It describes the functions of image intensifiers and flat panel detectors in converting x-ray energy into a visible light image for angiography. The learning objectives cover differentiating angiography from other exams, components of the angiography system, image modes, and factors controlling dose and image quality.