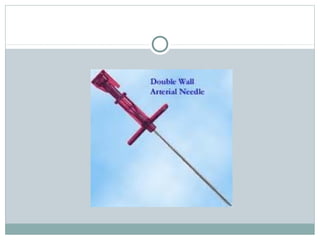
Interventional radiology uses minimally invasive techniques guided by imaging to diagnose and treat medical conditions. Procedures use small incisions or catheters inserted through blood vessels to access internal organs. The Seldinger technique is commonly used, involving insertion of a guidewire and catheter through a needle into the femoral artery. A variety of catheters and guidewires are used depending on the target vessel. Angiography involves injecting contrast dye to visualize vessels. Interventional radiology suites contain specialized equipment like large X-ray tubes and digital image receptors to facilitate complex image-guided procedures.