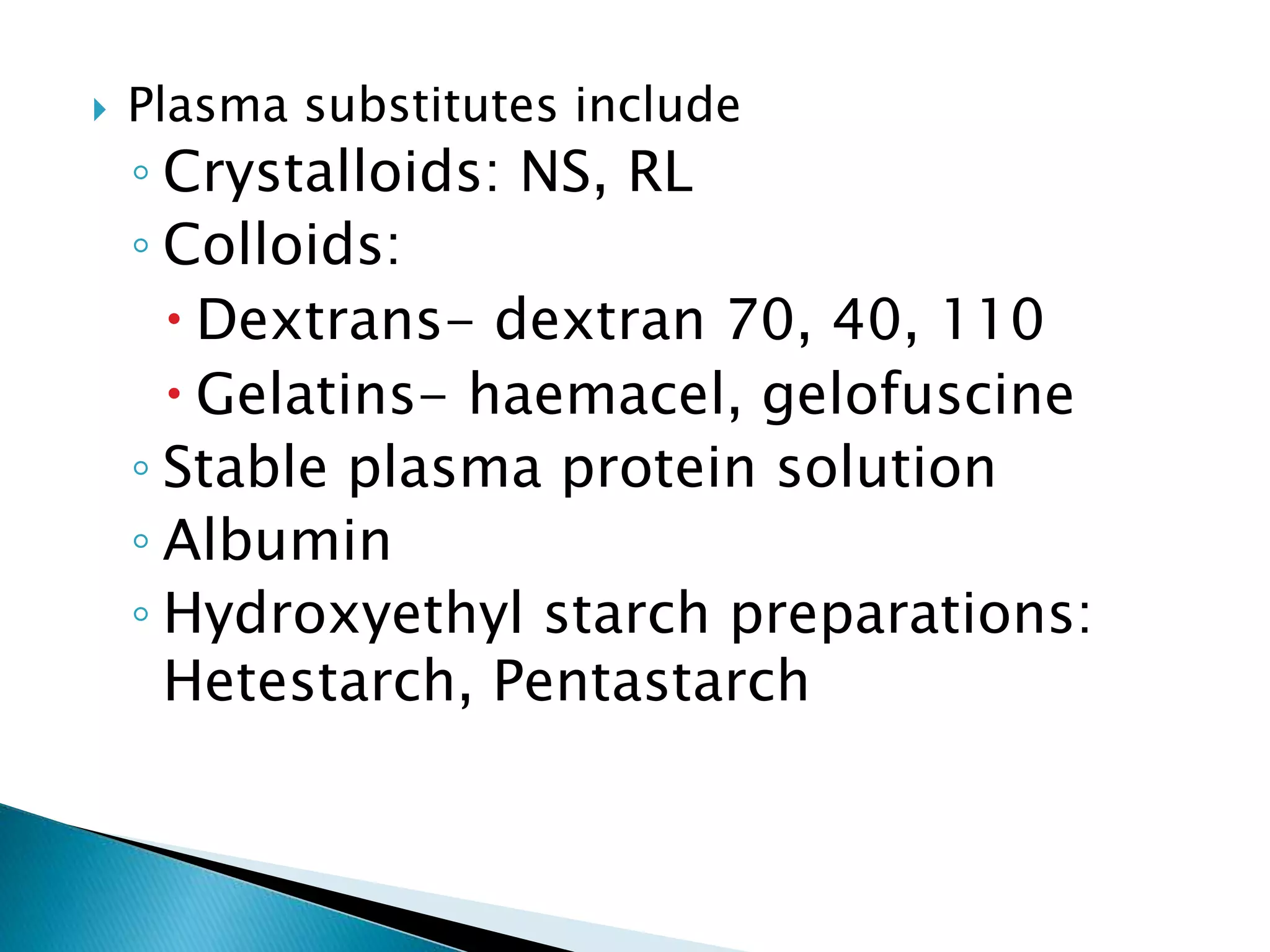
The document provides an overview of blood transfusion, including donor selection, blood components and their indications, pre-transfusion handling, administration principles, massive transfusion, autologous transfusion, complications and their management, and blood substitutes. Donor selection involves medical history screening and health assessments. Key blood components discussed are packed red blood cells, platelet concentrates, fresh frozen plasma, and cryoprecipitate. Proper storage, grouping, compatibility testing and administration procedures are outlined to ensure safety. Complications can be immediate or delayed, including infections transmitted and reactions to plasma proteins. Blood substitutes under development aim to replace functions of plasma, red cells and platelets.