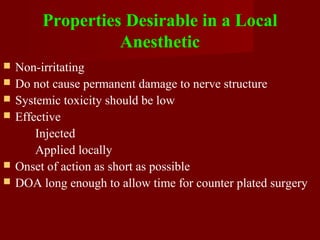
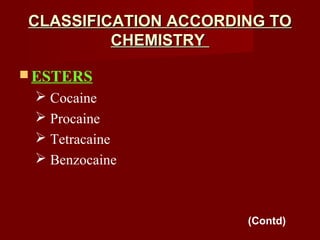
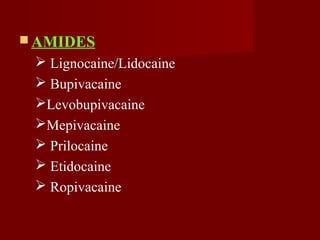
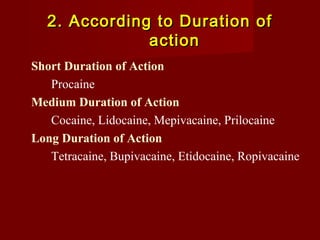
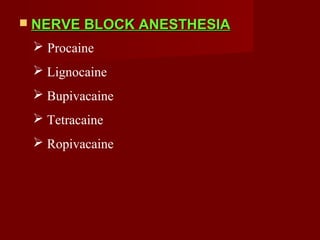
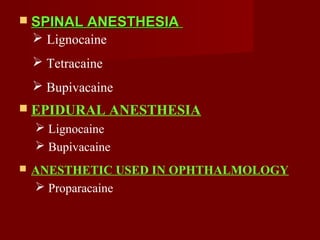
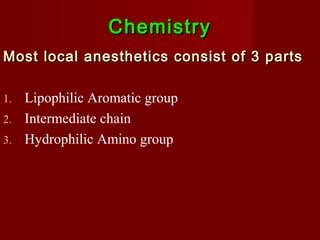
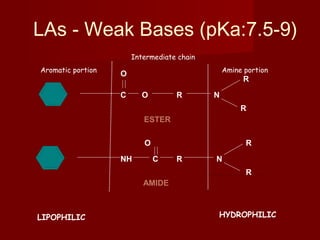
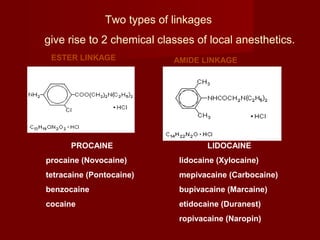
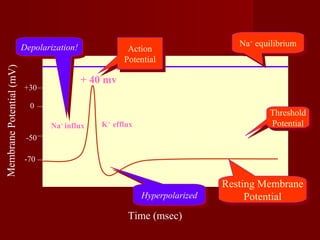
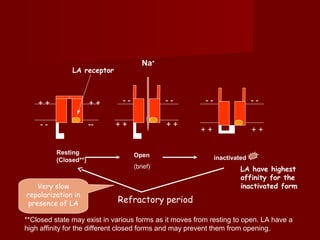
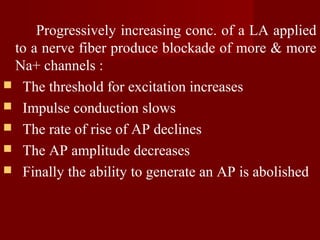
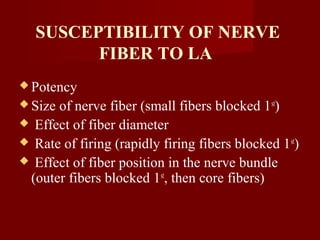
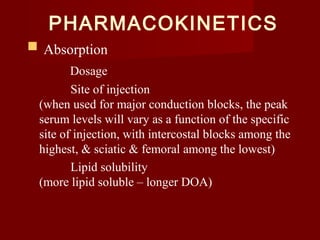
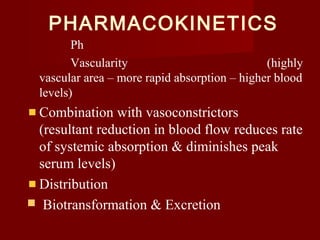
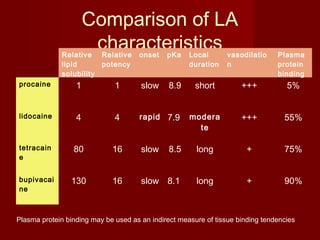
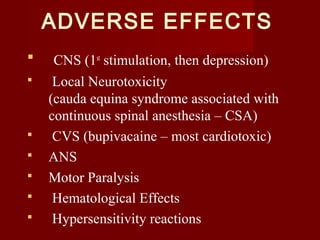
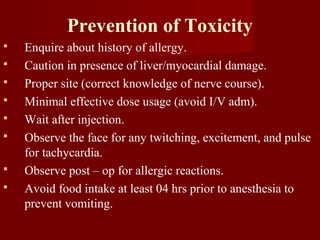
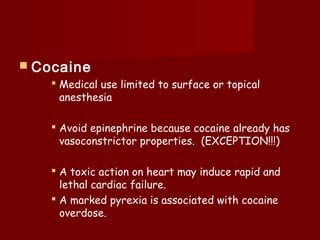
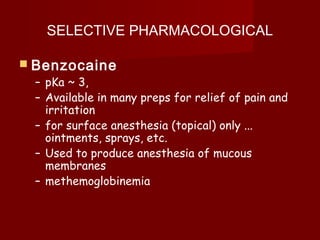
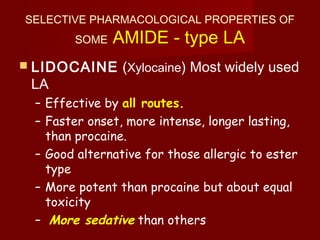
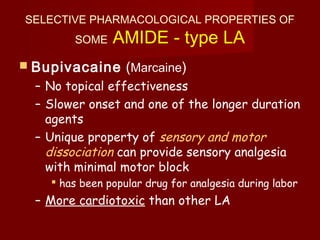
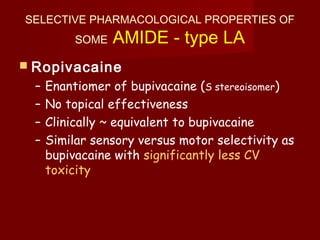
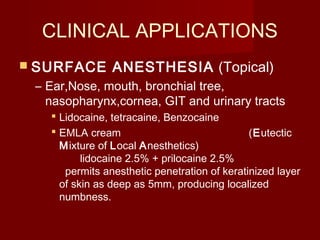
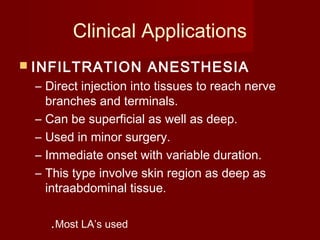
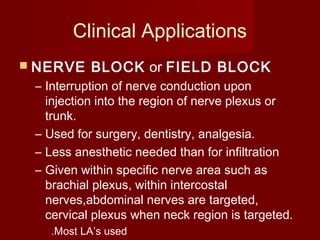
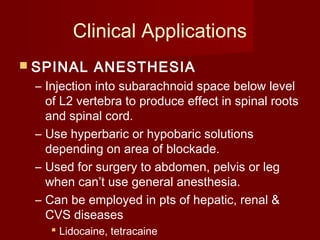
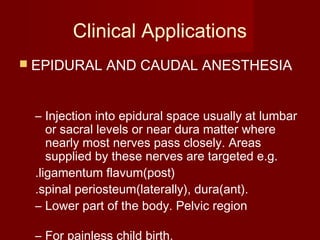
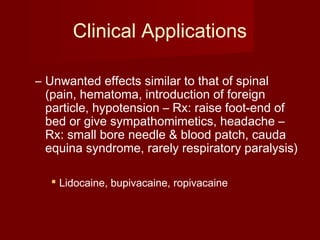
The document discusses local anesthetics, including their definition, classification, mechanisms of action, pharmacokinetics, clinical applications, and adverse effects. Specifically, it notes that local anesthetics reversibly block sodium channels to produce localized numbness, and are classified based on their chemical structure as esters or amides. Common examples like lidocaine, bupivacaine, and benzocaine are also mentioned.