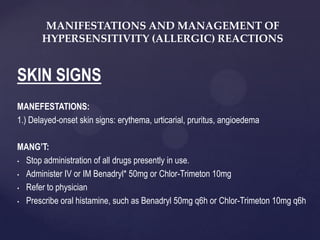
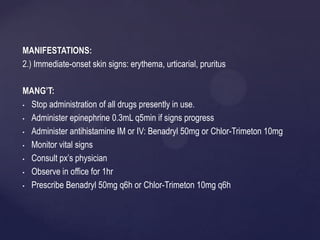
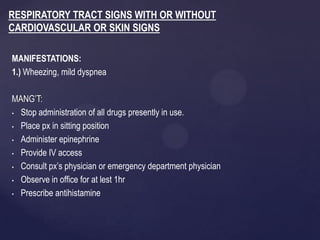
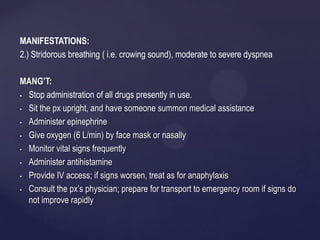
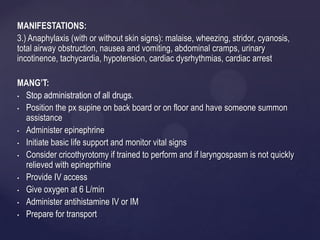
This document discusses allergic reactions and their management. It outlines various manifestations of allergic reactions involving the skin, respiratory tract, and anaphylaxis. Epinephrine is identified as the most important drug for treating allergic reactions. Symptoms involving breathing issues require immediate epinephrine administration to prevent death. Less severe reactions involving only rash or hives can be treated with antihistamines like Benadryl. It is important to always be prepared to treat anaphylaxis by having epinephrine readily available.