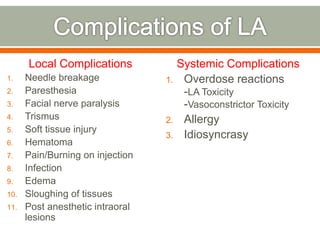
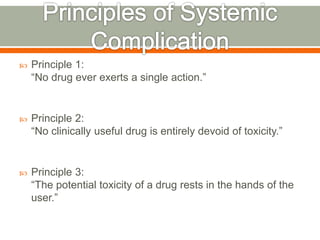
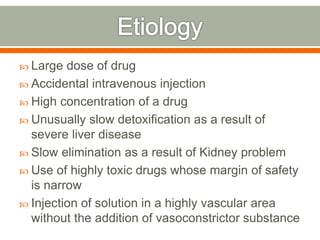
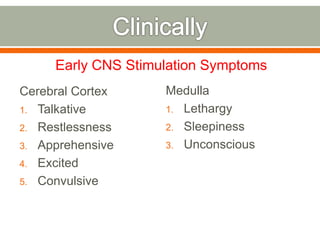
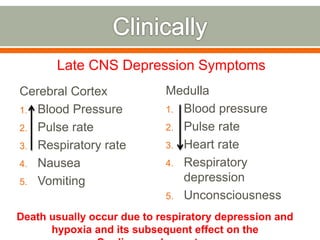
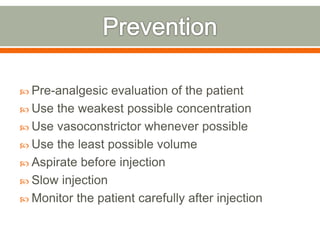
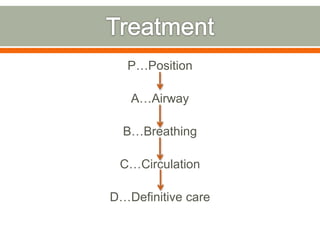
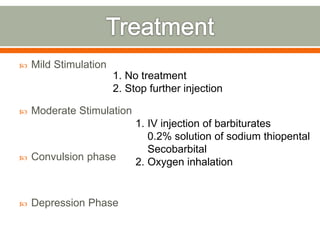
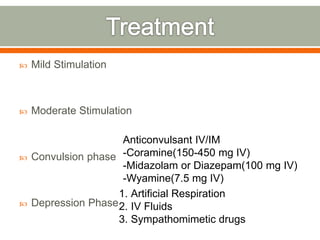
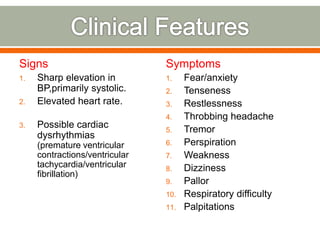
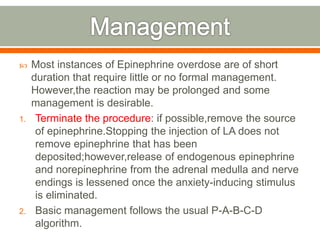
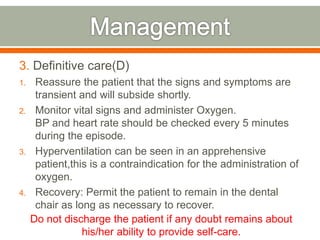
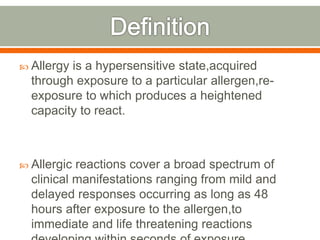
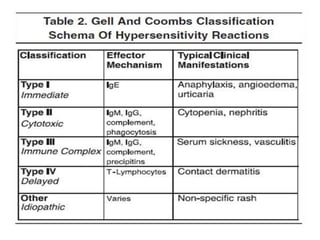
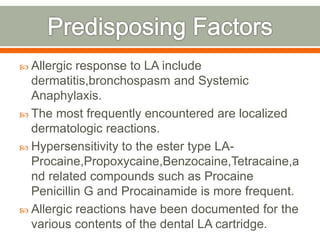
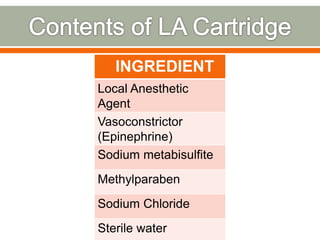
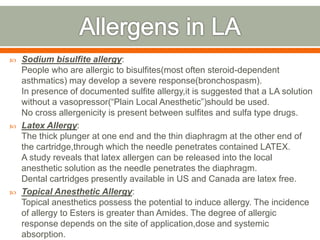
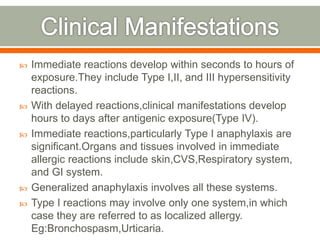
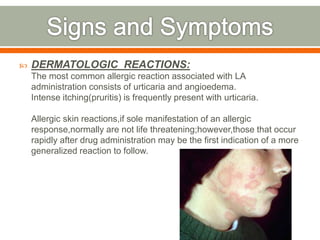
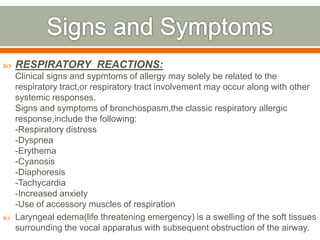
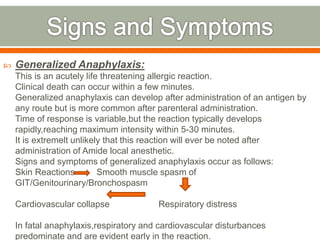
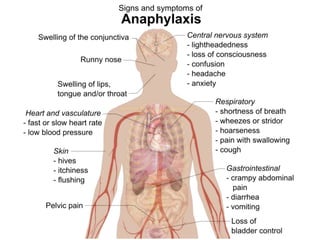
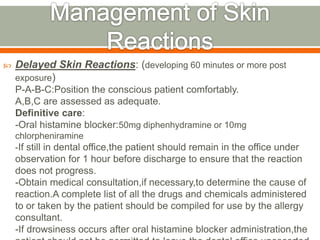
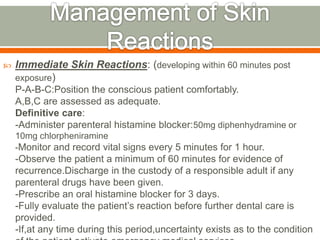
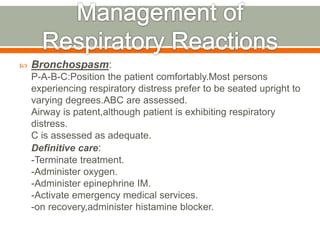
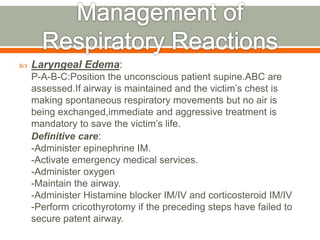
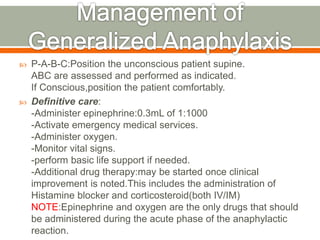
The document discusses local anesthesia and its potential complications. It defines local anesthesia and lists local and systemic complications. It discusses the principles of drug toxicity and the role of the user in potential toxicity. It describes overdose reactions involving the central nervous system and treatments. It provides guidelines for safe administration of local anesthesia and managing complications like overdose reactions and allergic responses.