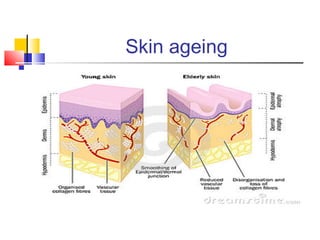
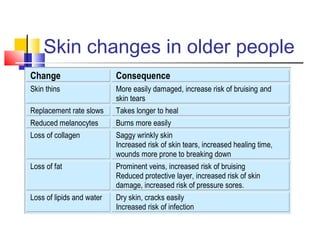
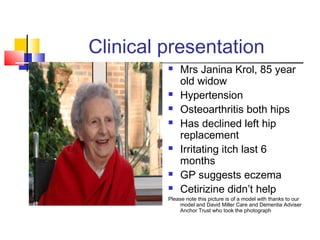
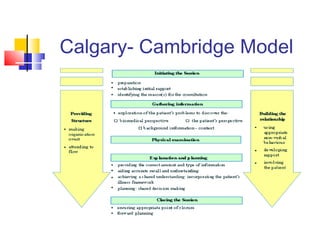
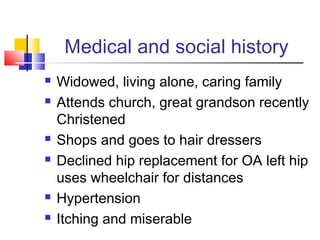
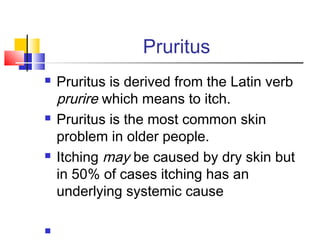
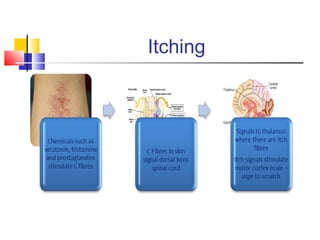
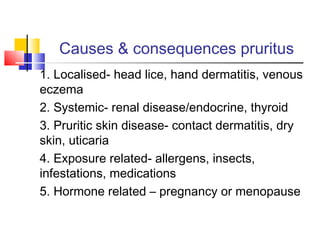
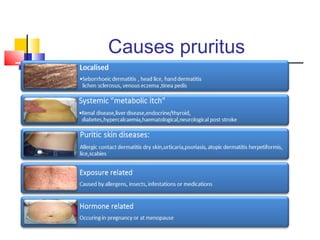
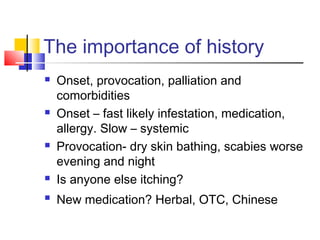
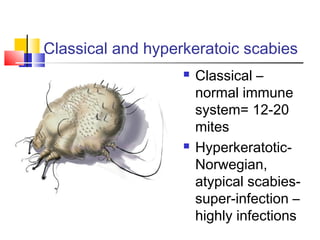
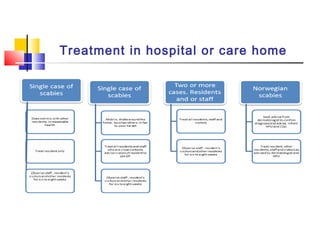
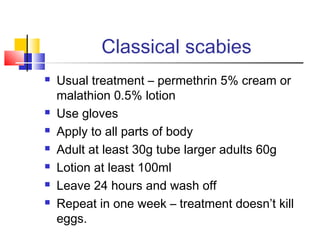
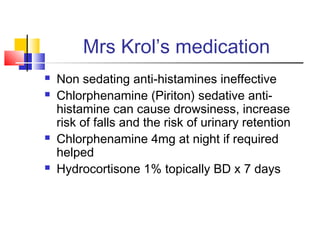
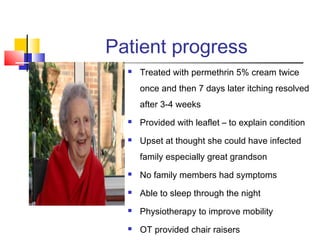
This document discusses dermatological problems in older people, with a focus on pruritus (itching). It provides information on how aging affects the skin and increases vulnerability to conditions. It then presents a case study of an 85-year-old woman experiencing itching for 6 months. Through examination, the diagnosis of scabies is determined. Scabies is described, including transmission, symptoms, diagnosis via microscopy, and treatment guidelines. The patient is successfully treated with topical permethrin cream and antihistamines, resolving her itching and allowing her improved sleep and quality of life. The value of nurses properly diagnosing and treating such conditions is emphasized.