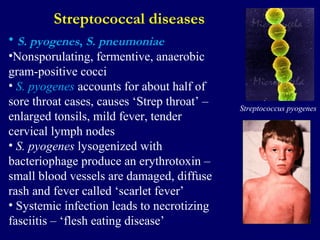
The document discusses various microorganisms found in air, including bacteria and viruses. It notes that microorganisms can exist up to 1000 feet above the Earth's surface attached to particles, and that dry weather leads to a higher microbial load in air while wet weather washes microorganisms out of the air. It then summarizes several pathogenic bacteria and viruses that are transmitted via the air or respiratory routes, such as Streptococcus, diphtheria, pertussis, tuberculosis, influenza, and their effects on human health.