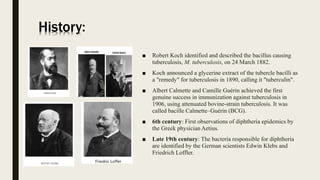
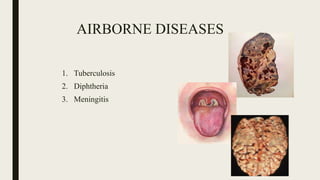
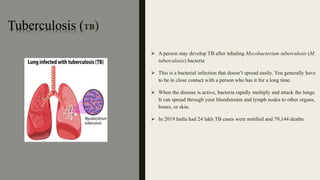
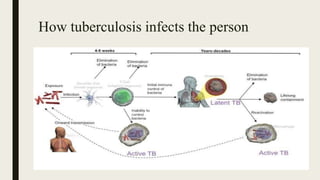
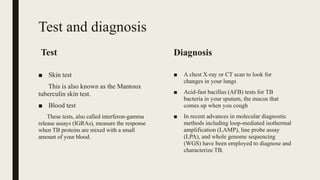
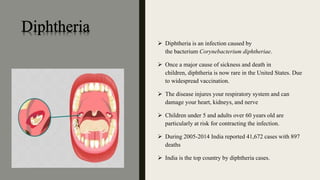
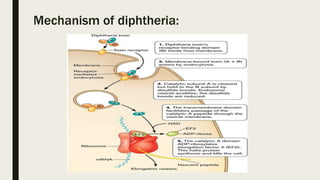
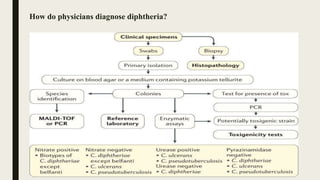
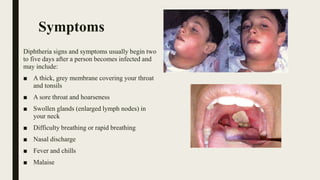
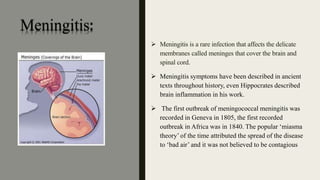
This document discusses several airborne diseases including tuberculosis, diphtheria, and meningitis. It provides background on the history and transmission of each disease. Tuberculosis is caused by bacteria that can be inhaled from an infected individual. It most commonly affects the lungs. Diphtheria is caused by bacteria that can spread through coughing or sneezing. Meningitis has several causes including bacteria, viruses, and fungi, and it inflames the membranes surrounding the brain and spinal cord. Prevention of airborne diseases focuses on good hygiene practices like handwashing and covering coughs and sneezes.