The document discusses various topics related to disease transmission and infection control including:
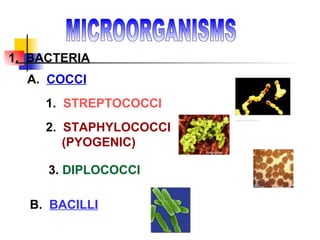
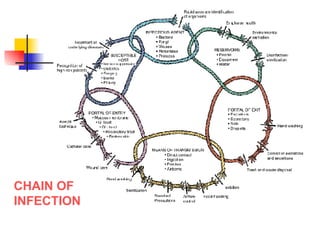
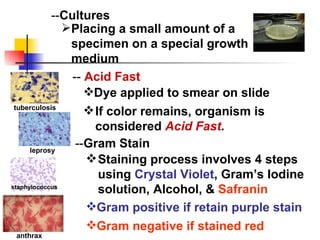
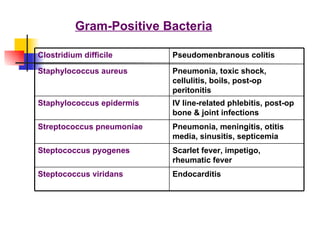
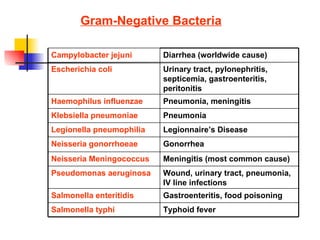
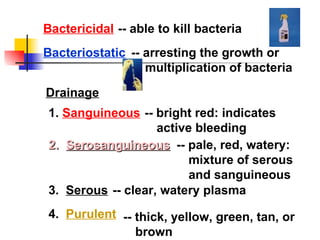
1. Different types of microorganisms that can cause disease such as bacteria, viruses, fungi.
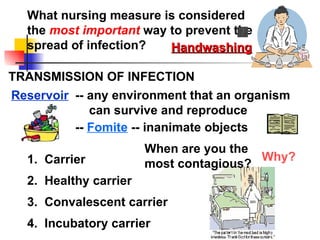
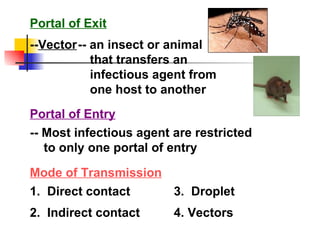
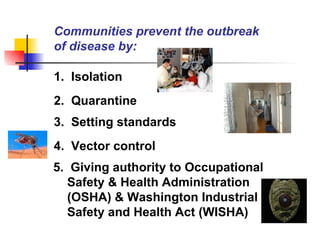
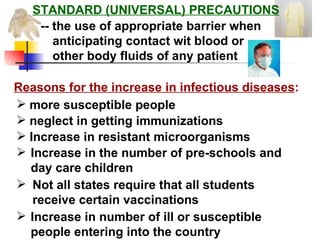
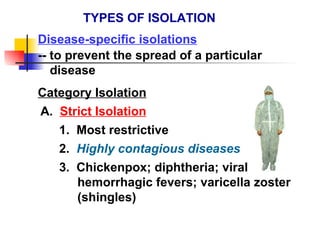
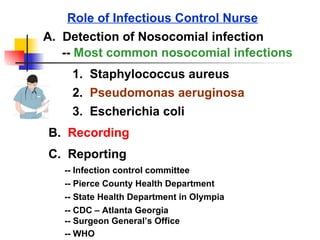
2. Methods of sterilization and ways to prevent the spread of infections like isolation and standard precautions.
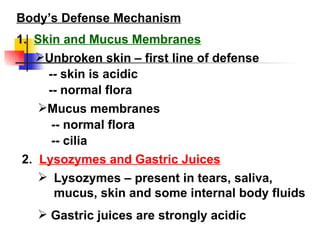
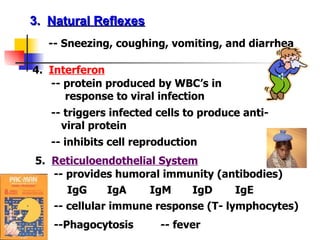
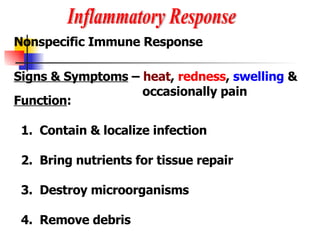
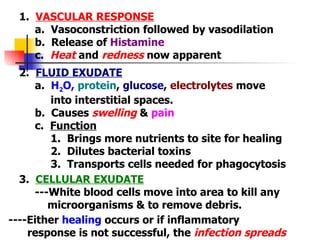
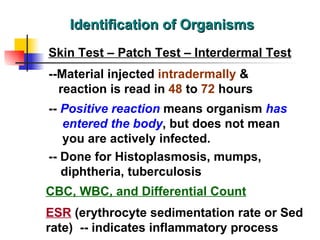
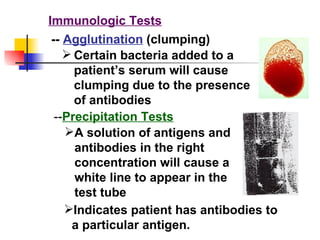
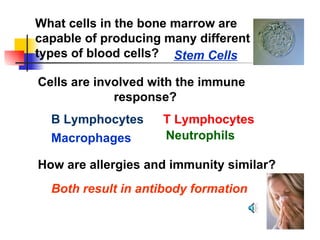
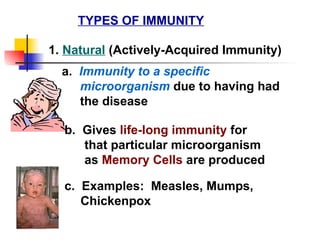
3. The body's defense mechanisms against pathogens including physical barriers, inflammation, and the immune response.