1. Venovenous extracorporeal membrane oxygenation (VV ECMO) is a rescue therapy for severe acute respiratory distress syndrome (ARDS) with high mortality rates. It allows the lungs to rest and heal while providing oxygenation to the blood.
2. Modern VV ECMO circuits are safer and more effective than older models, using improved oxygenators, pumps, and often dual lumen cannulas. Patients supported with VV ECMO have survival rates around 60% according to the ELSO registry.
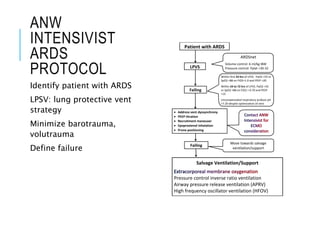
3. Providing effective VV ECMO requires a highly skilled multidisciplinary team and standardized protocols. Key challenges include properly selecting patients, ventilator management to rest the lungs, and coordin