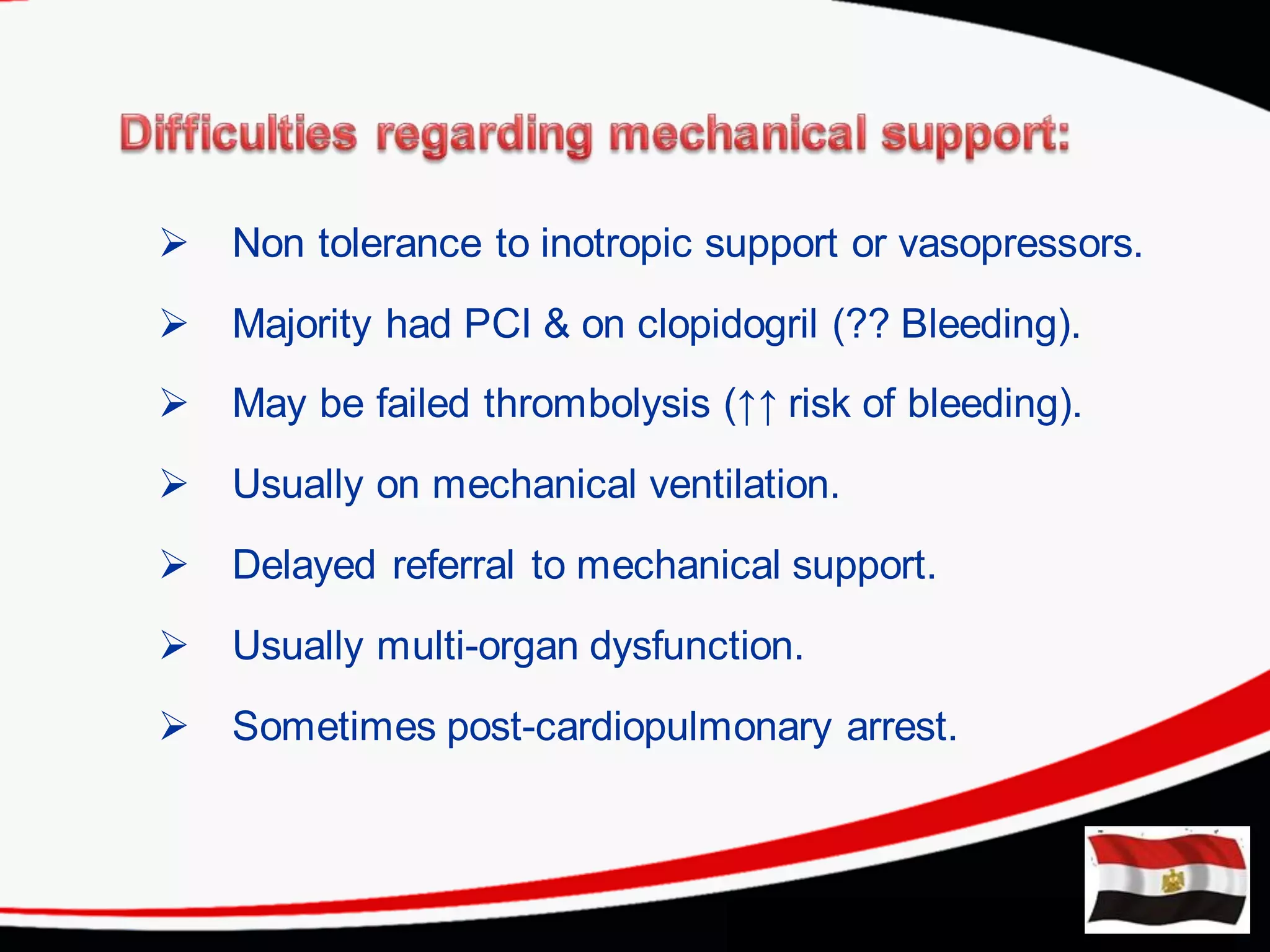
The document discusses cardiogenic shock's definition, causes, and management strategies, emphasizing the need for timely intervention with mechanical support systems like IABP, ECMO, and Impella devices. It highlights the critical clinical indicators to evaluate the need for these devices, the complications associated with each method, and the effectiveness of ECMO in cases of acute refractory cardiac failure. Ultimately, it underscores the importance of understanding patient status and appropriate device selection to improve survival rates in cardiogenic shock cases.