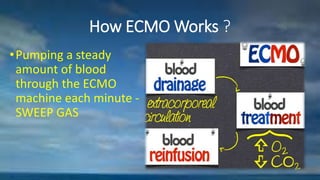
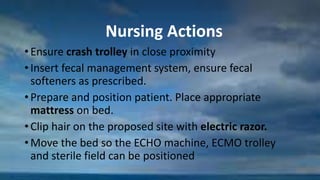
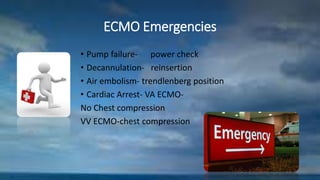
ECMO is a form of life support that takes over the work of the heart and lungs by pumping and oxygenating blood outside of the body. It can provide temporary support to allow the heart and lungs time to rest and recover from injury or illness. Key components are cannulas placed into major veins or arteries to drain and return blood, an oxygenator to add oxygen and remove carbon dioxide, and a pump to circulate blood through the system. An ideal ECMO team includes physicians, perfusionists, nurses and respiratory therapists who carefully monitor the patient and equipment to address any complications and manage the patient through the course of support and weaning off ECMO.