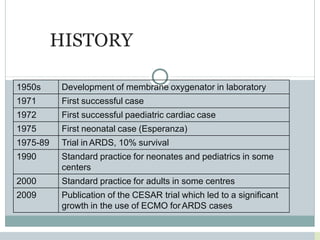
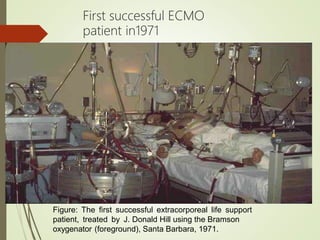
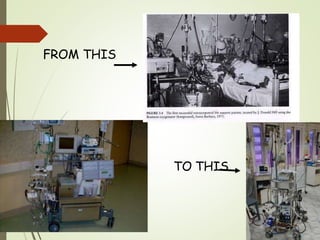
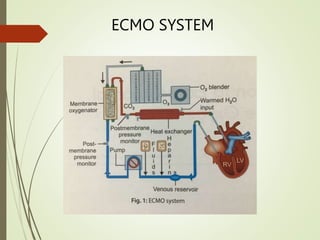
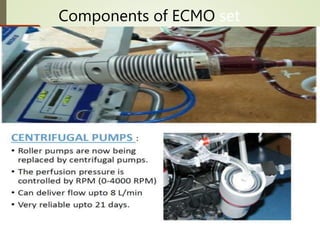
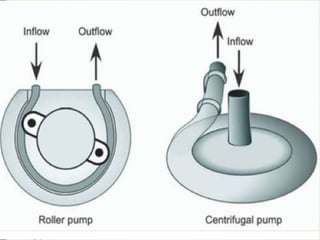
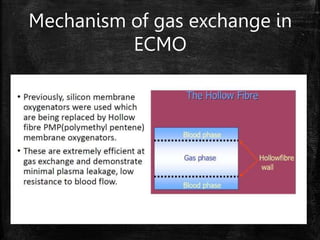
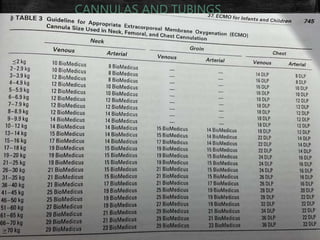
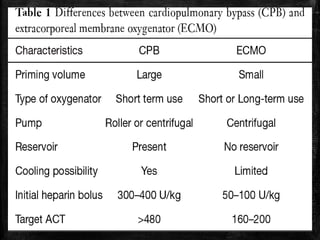
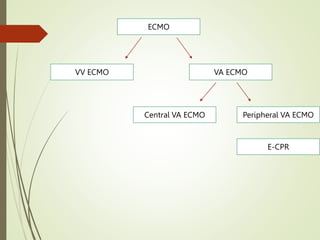
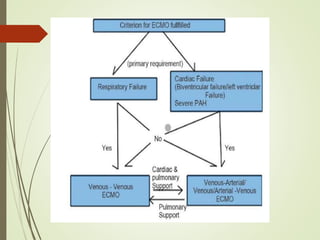
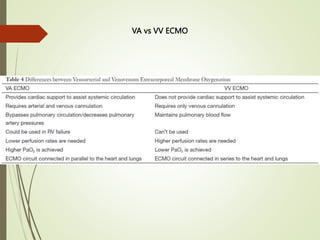
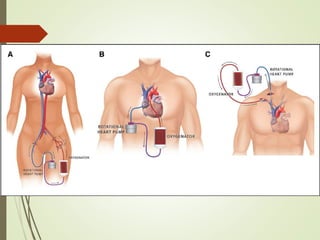
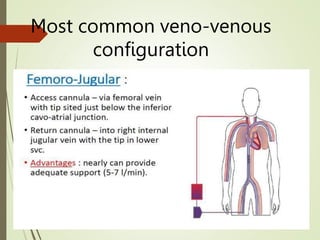
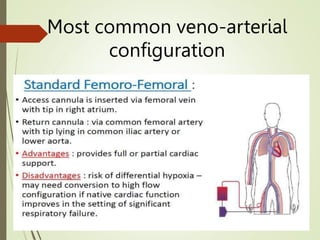
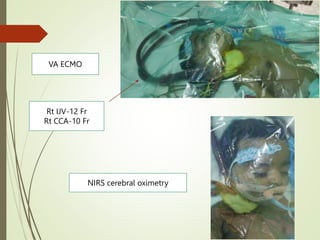
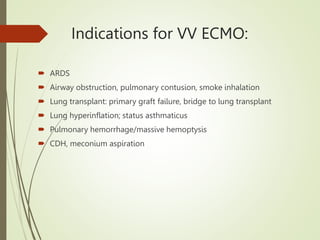
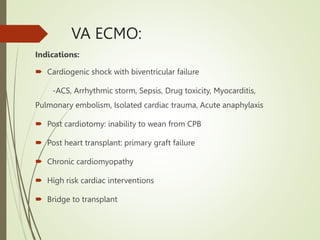
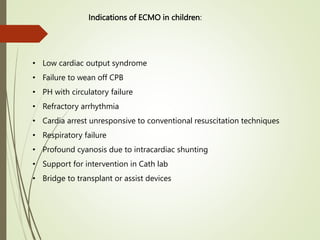
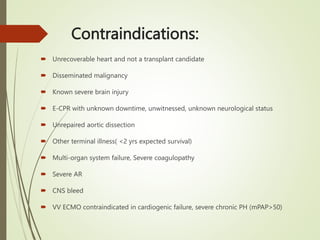
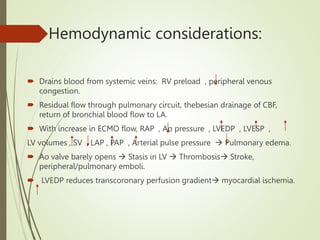
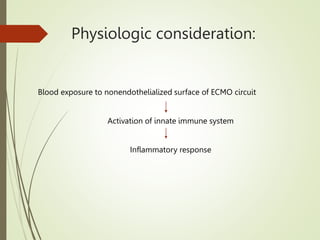
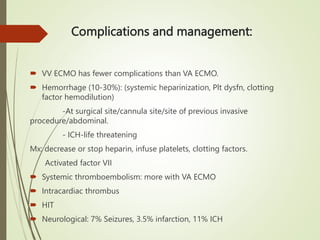
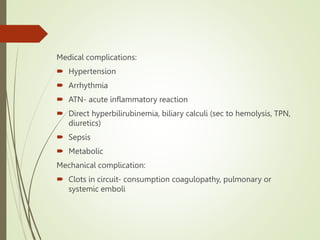
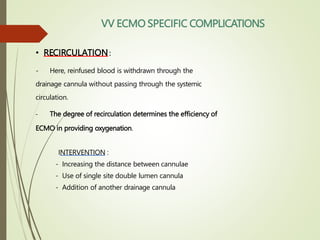
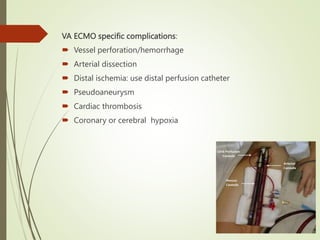
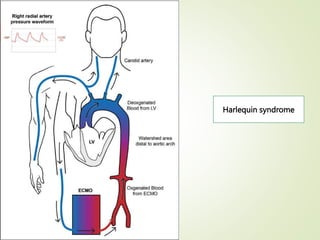
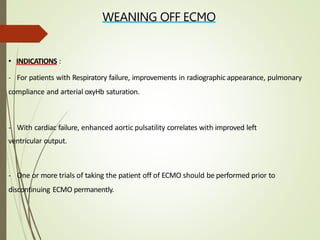
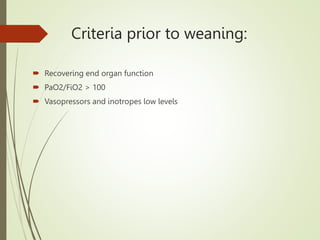
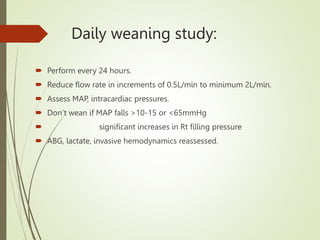
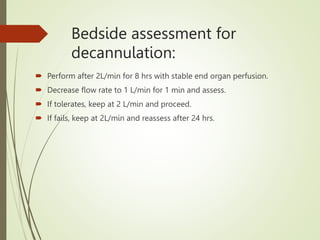
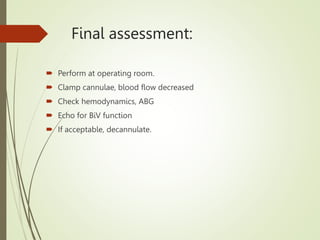
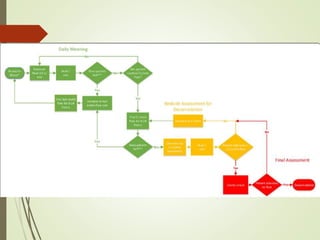
ECMO is a form of extracorporeal life support used for patients with severe cardiac or respiratory failure. It works by removing blood from the body, oxygenating it, and returning it. The document discusses the history and development of ECMO, components of the ECMO circuit, modes of ECMO including veno-venous and veno-arterial, indications and contraindications for its use, complications, and criteria for weaning patients off of ECMO support.