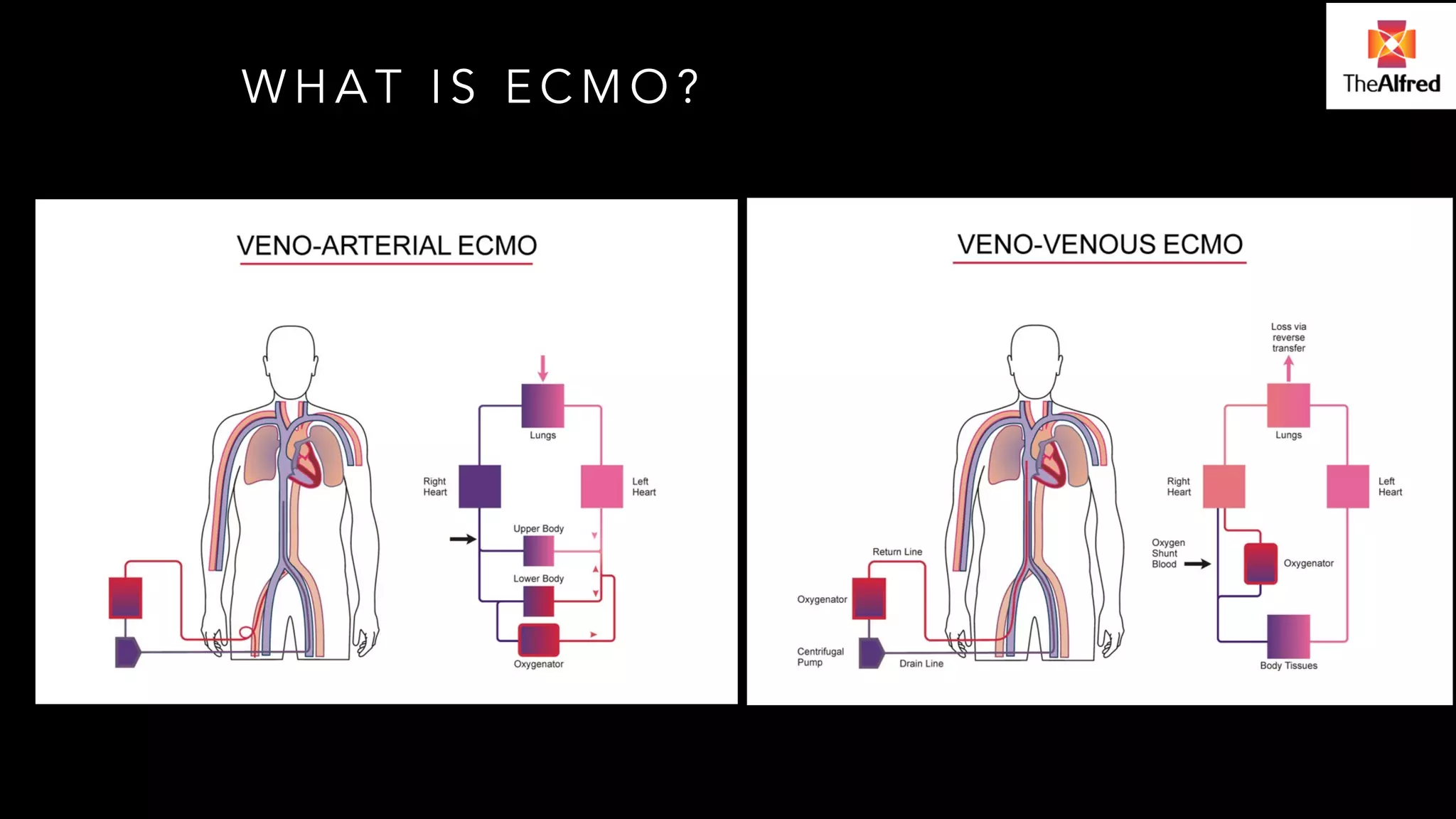
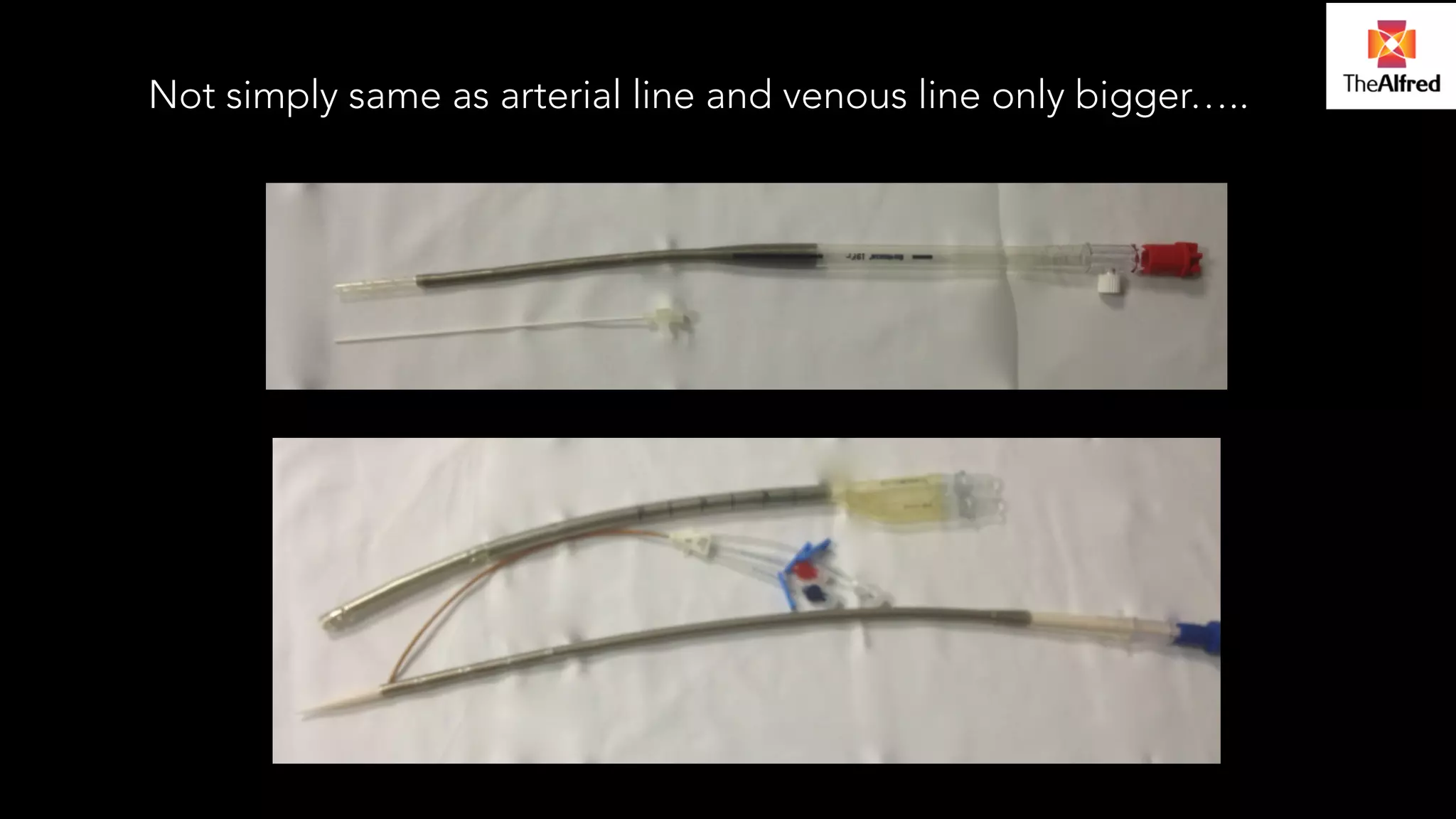
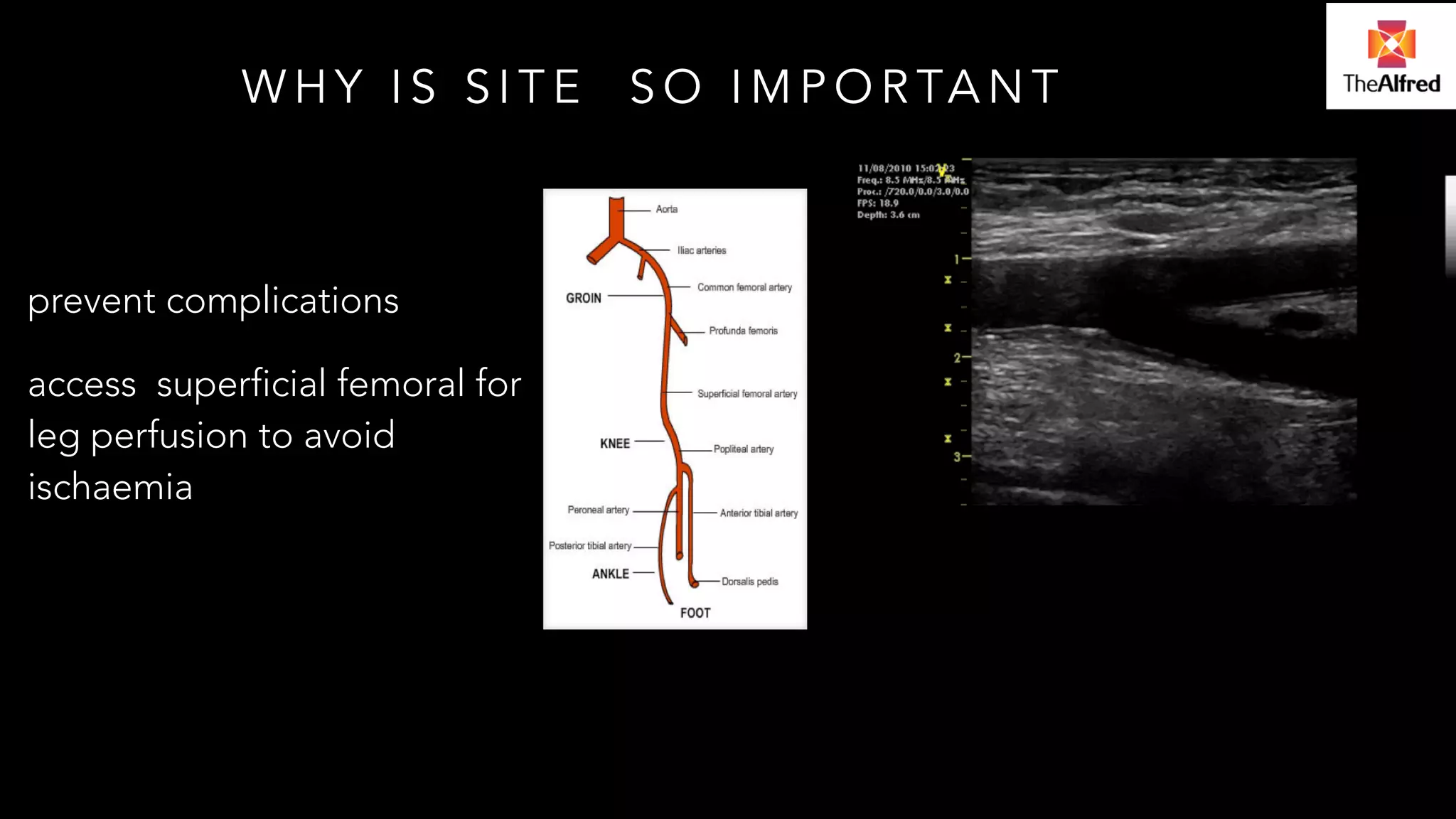
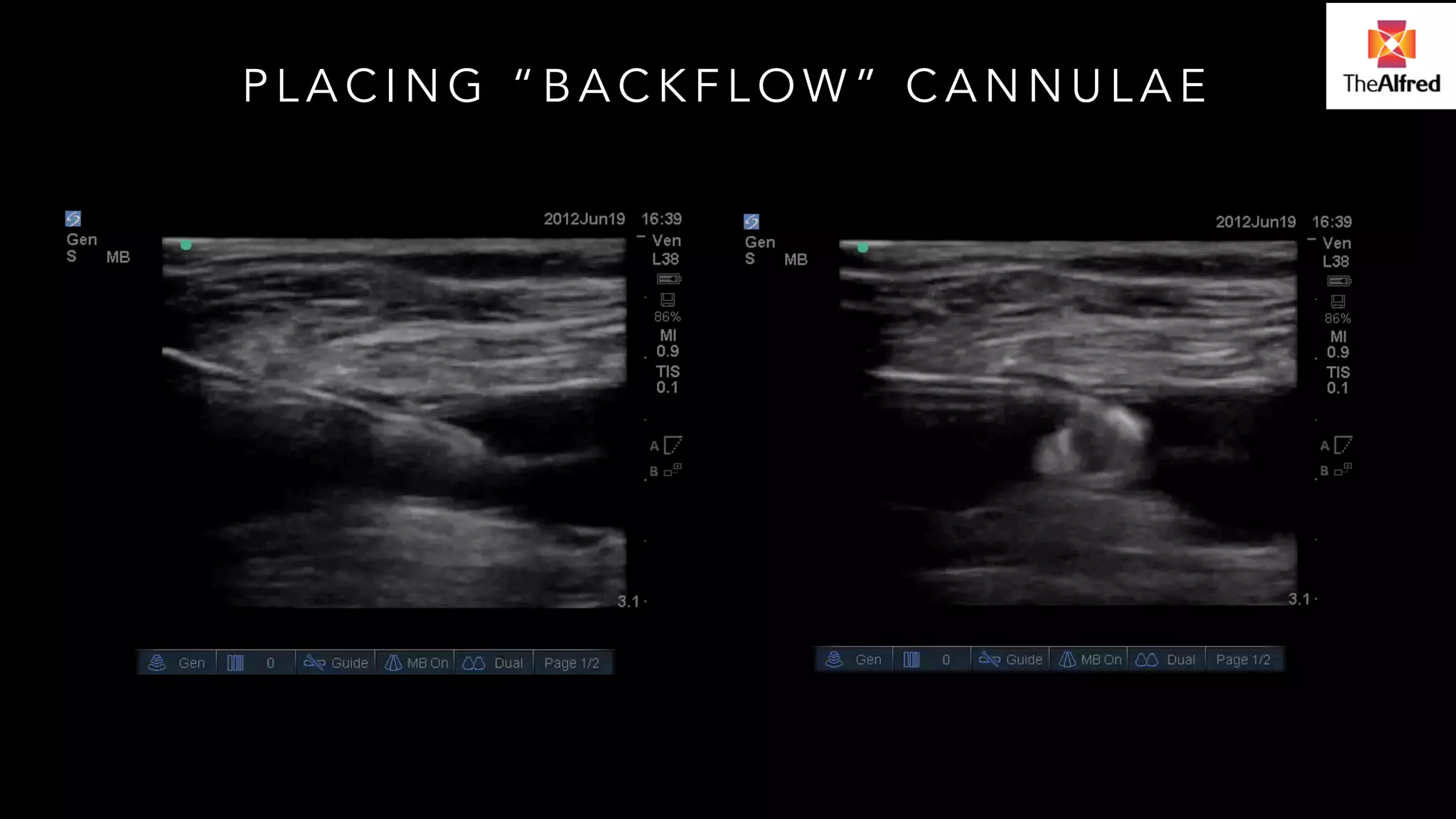
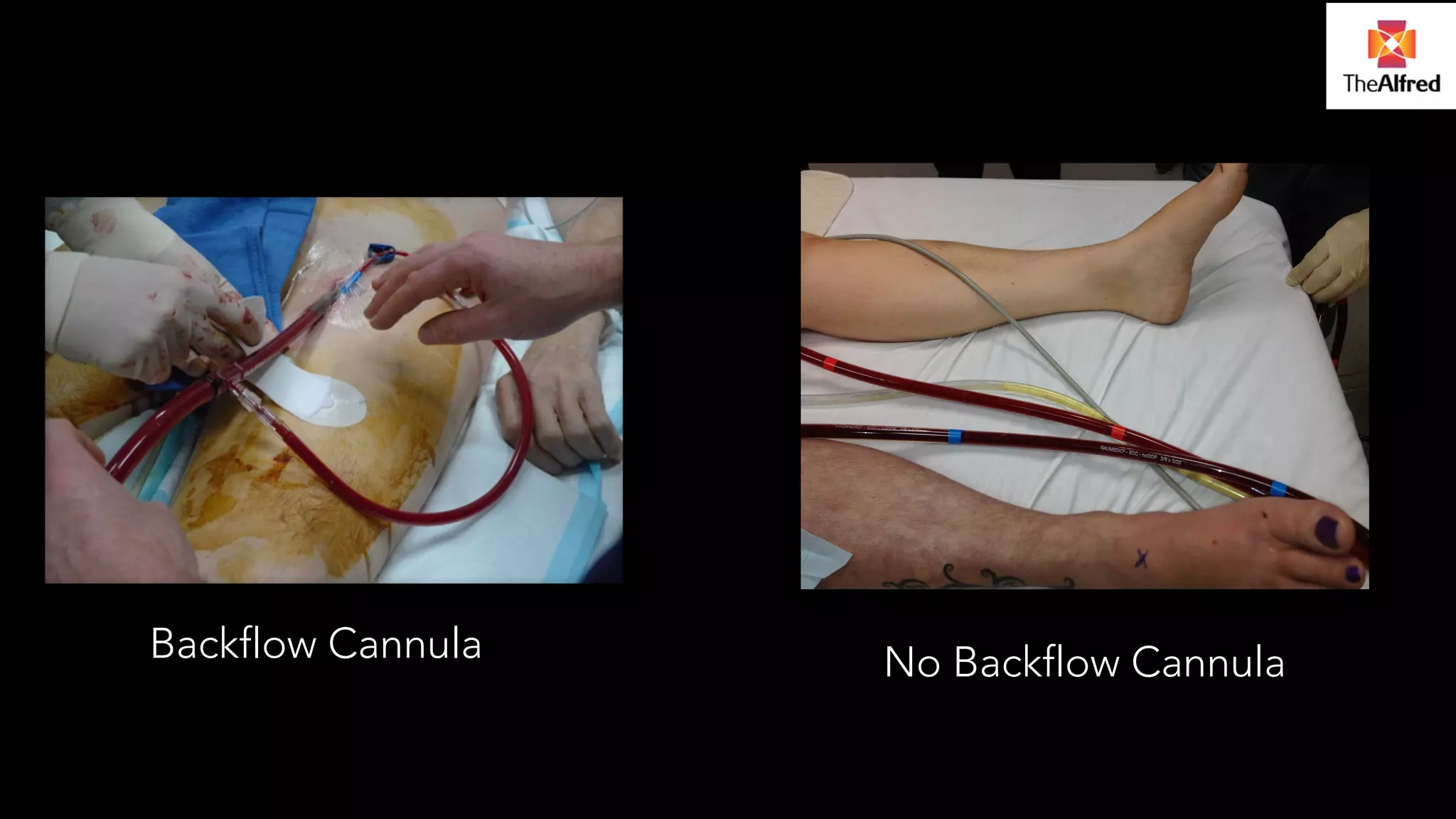
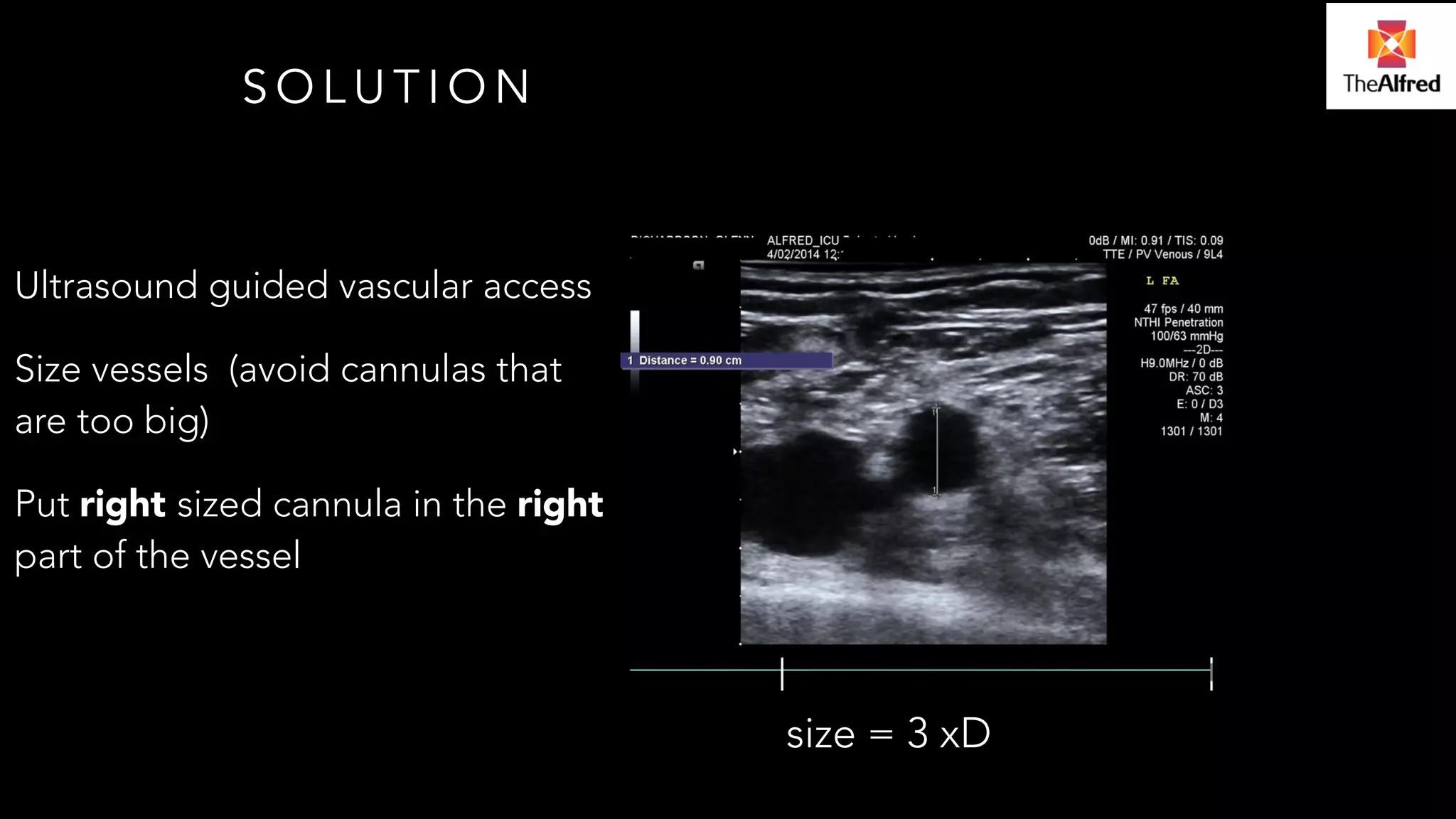
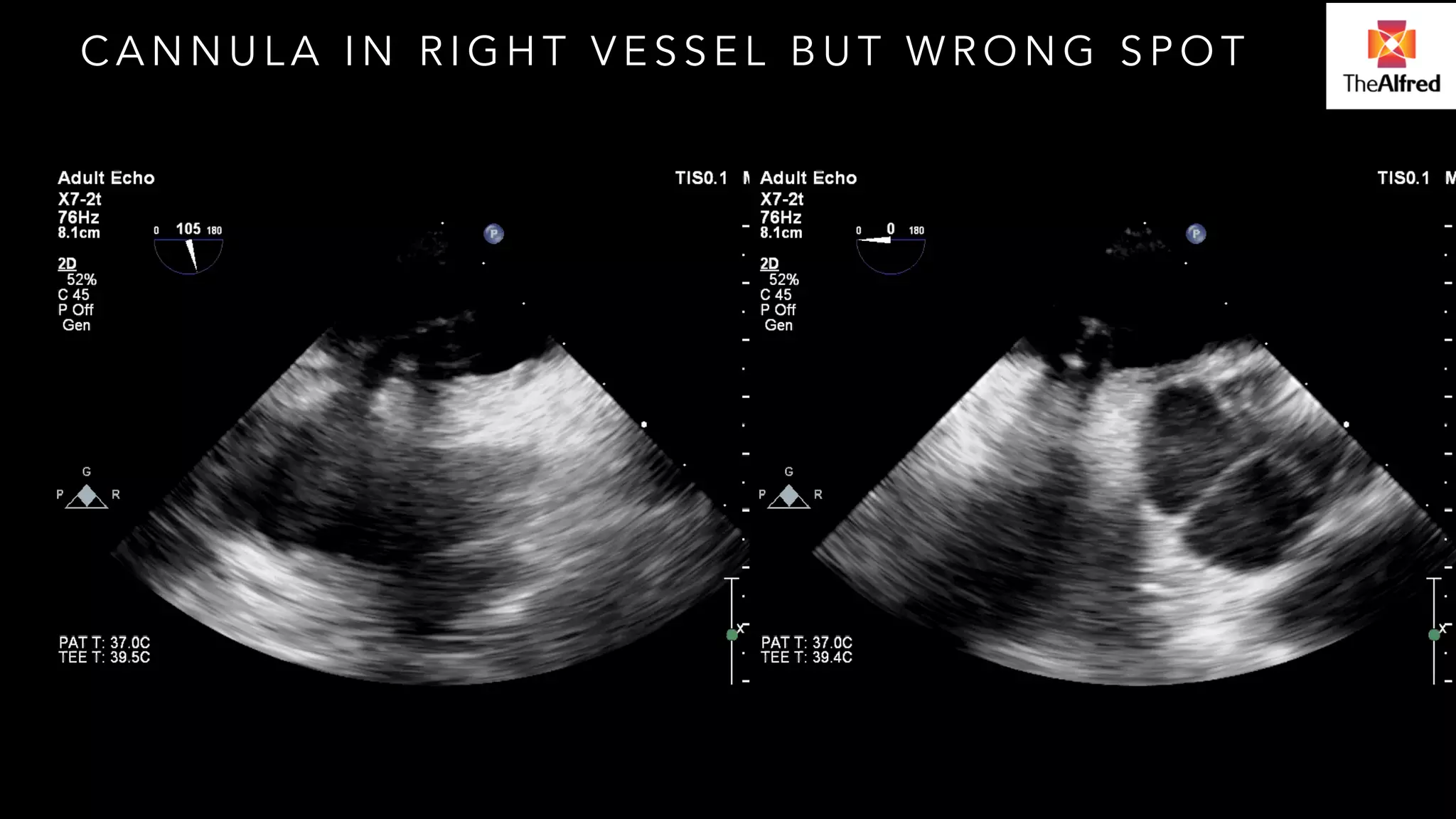
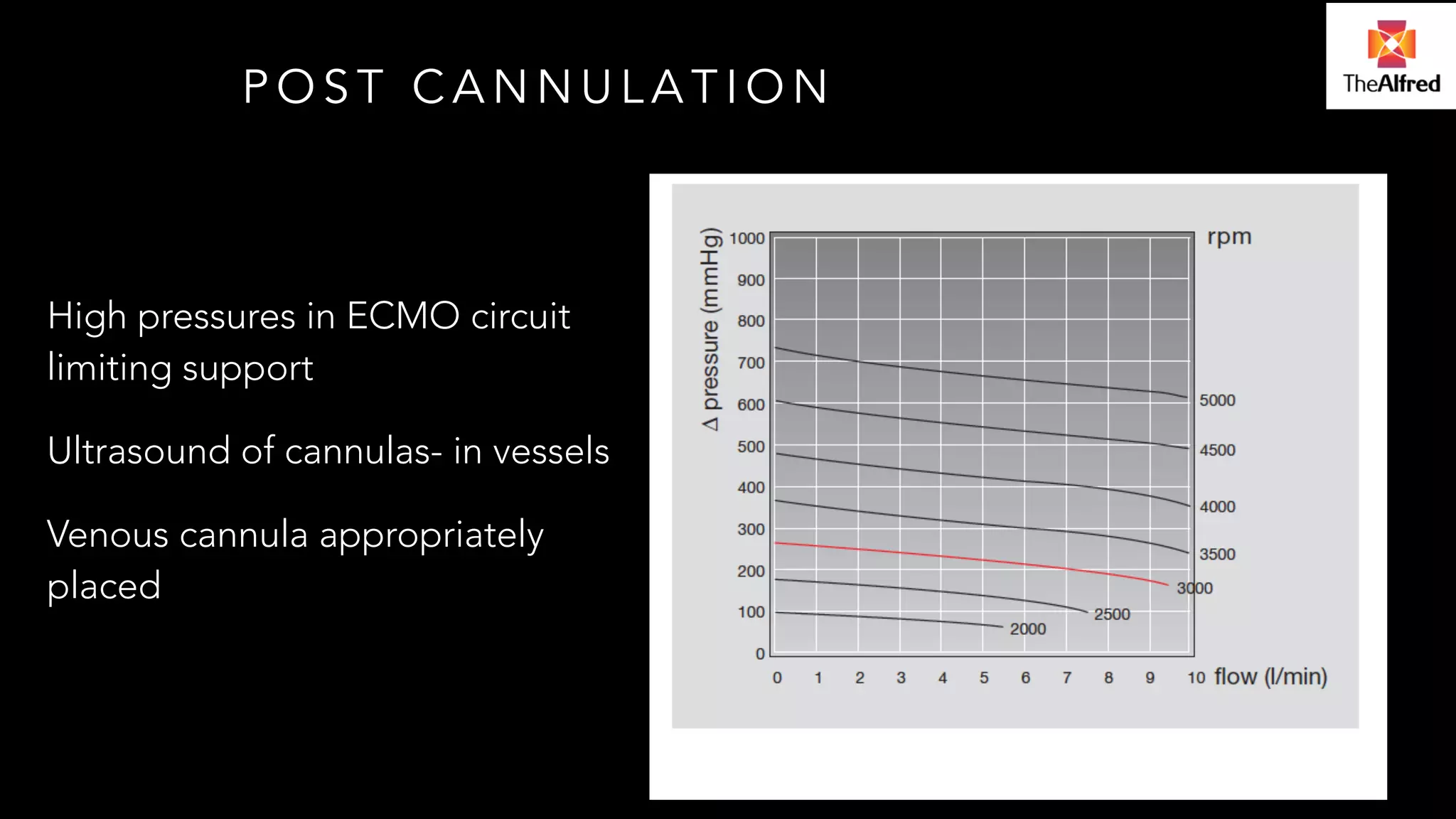
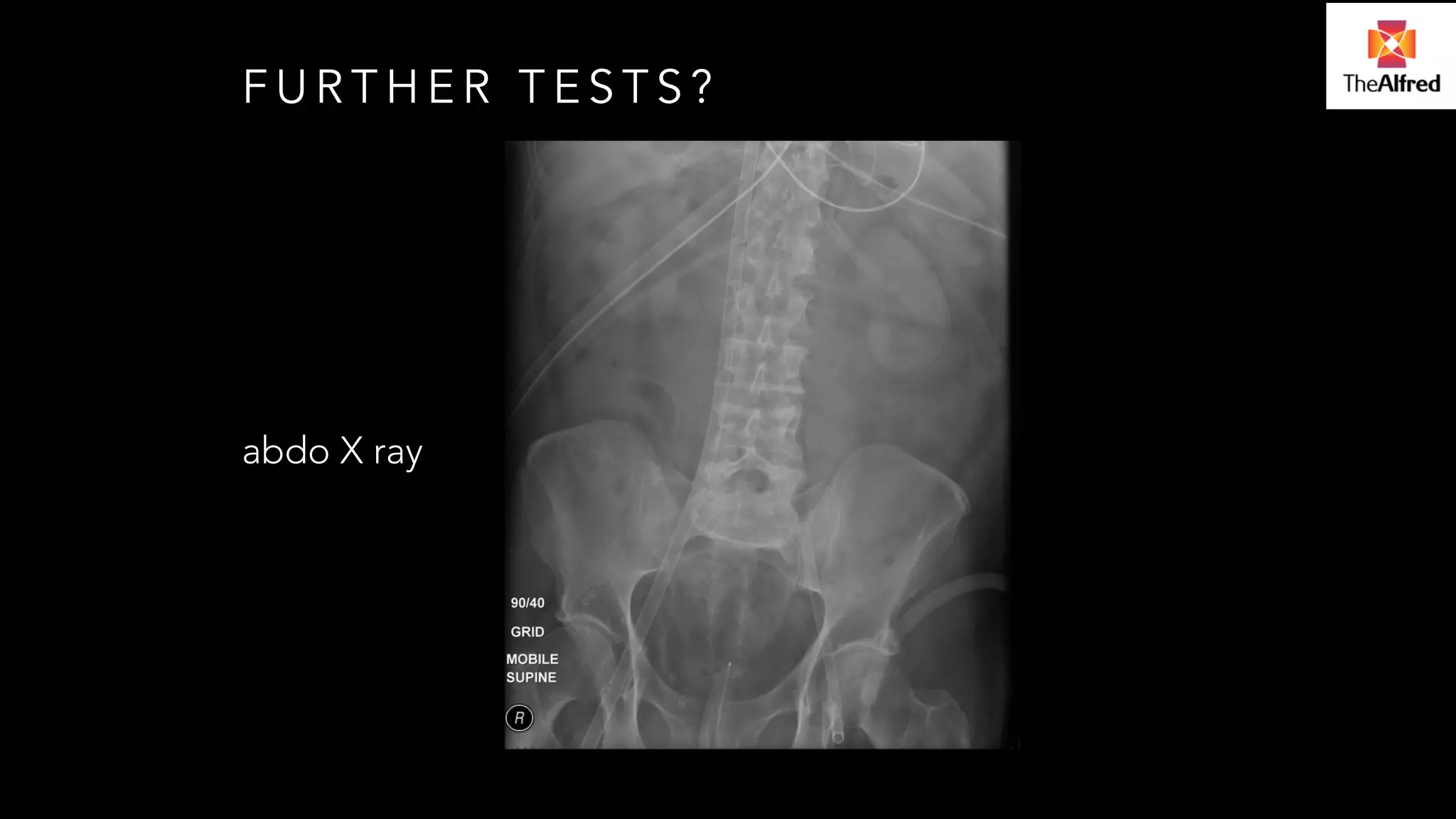
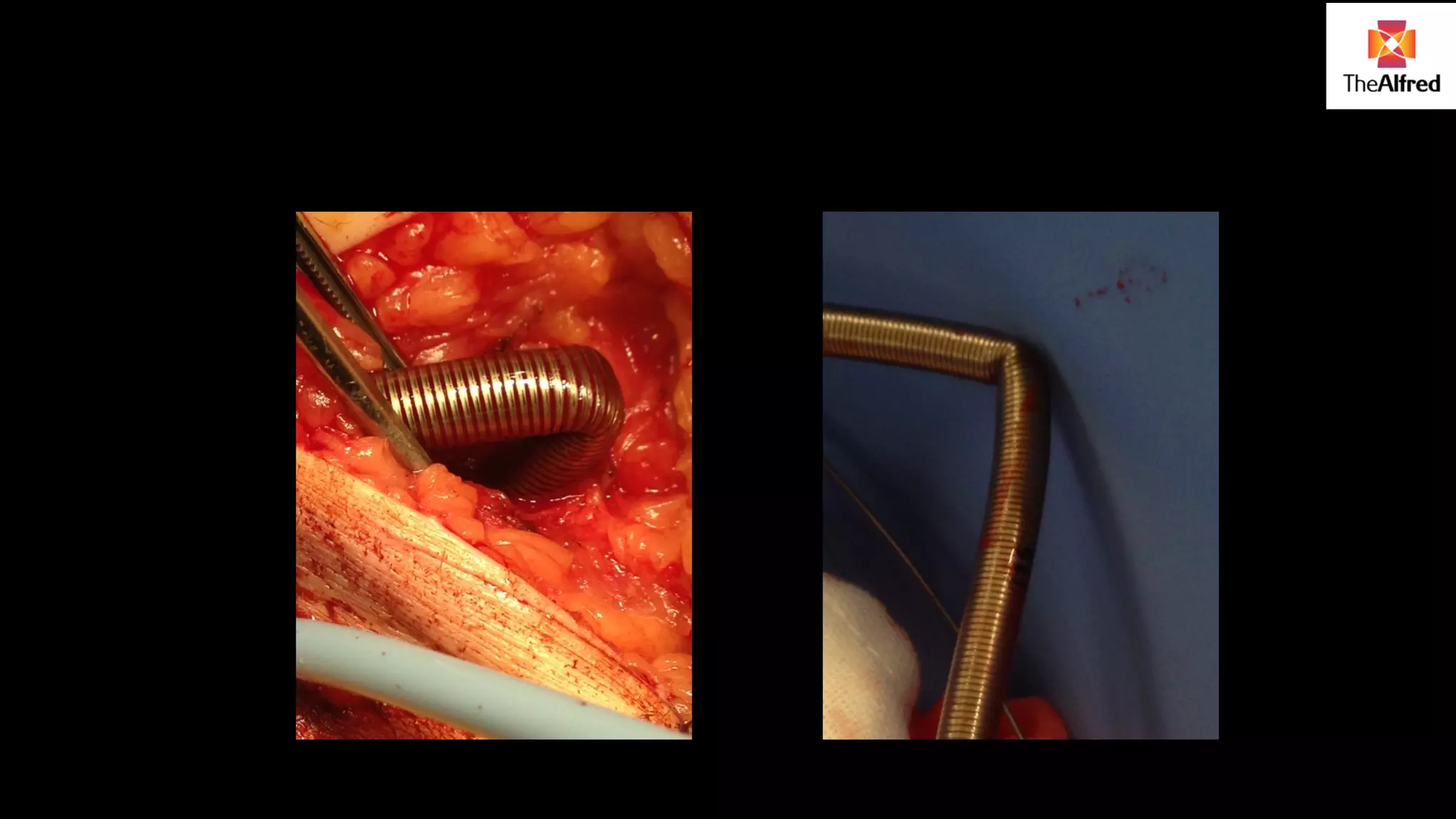
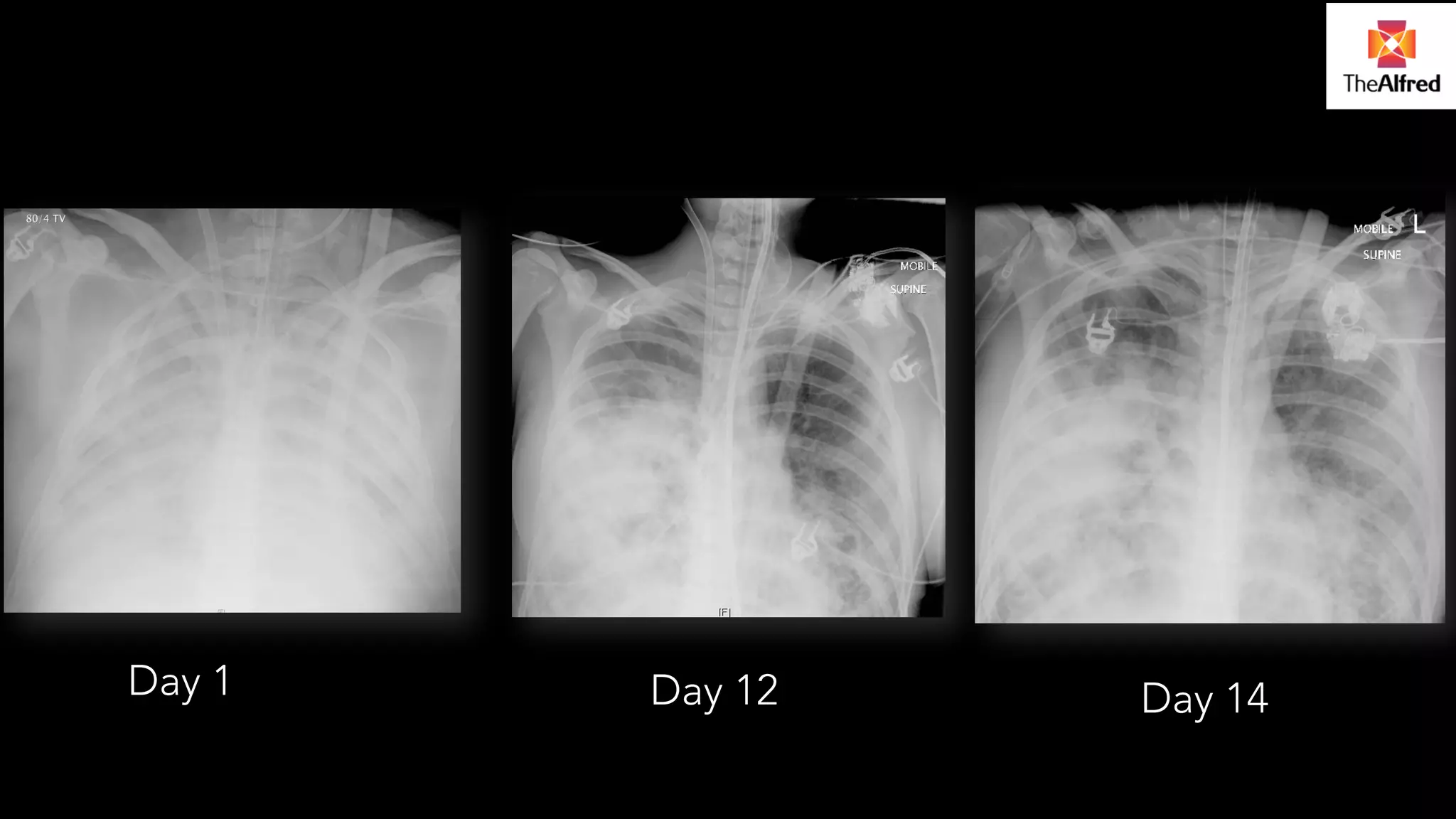
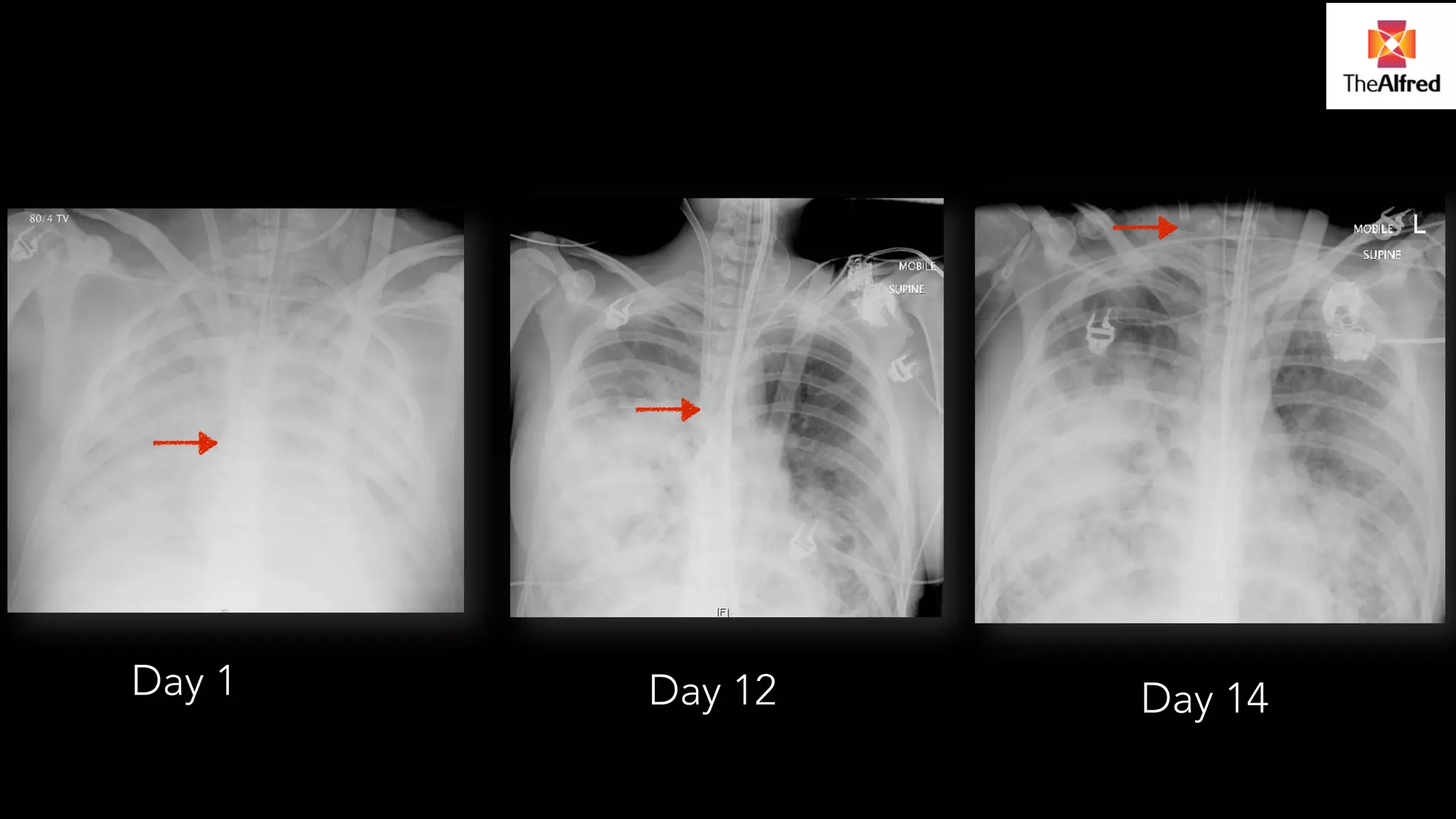
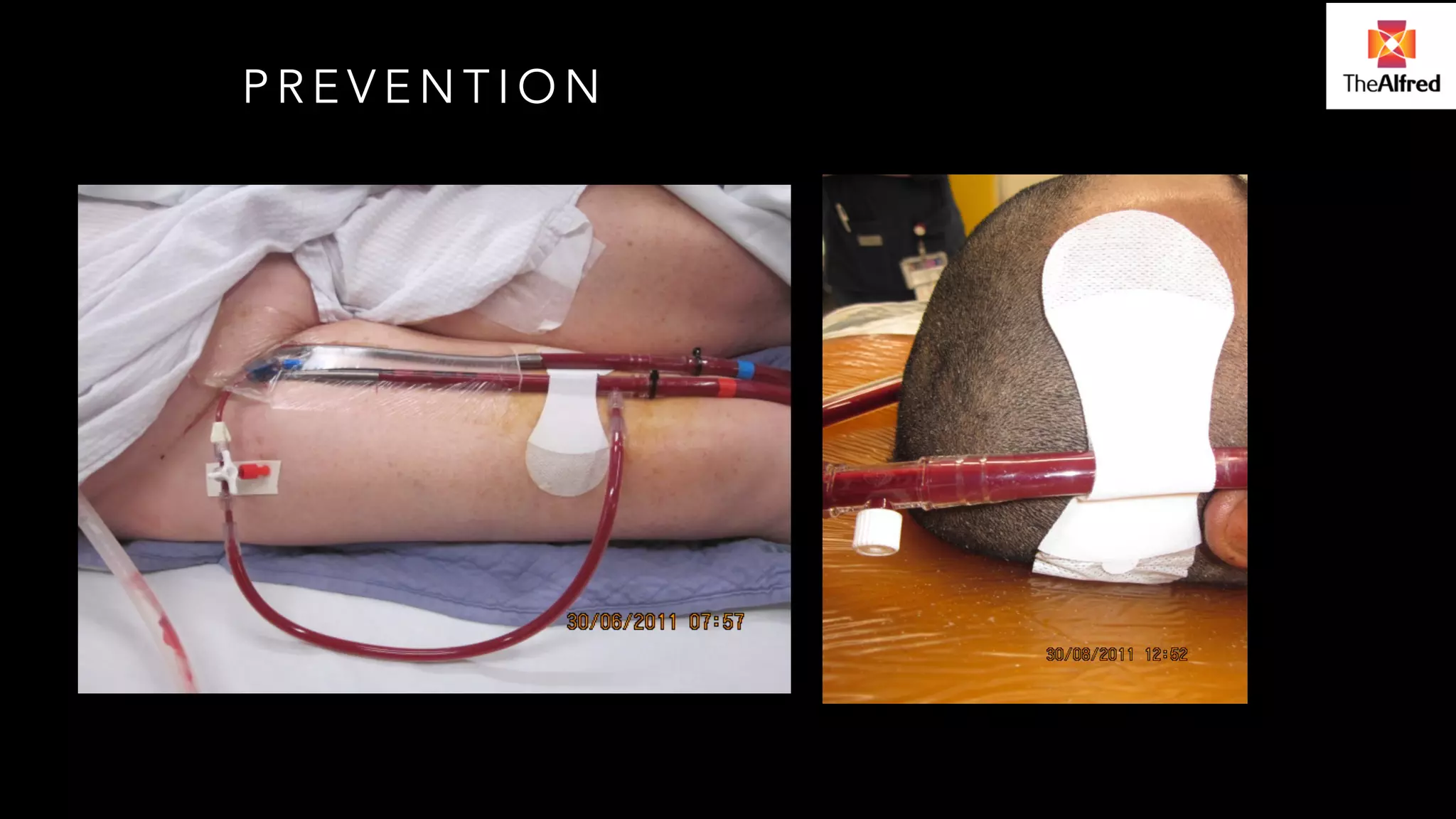
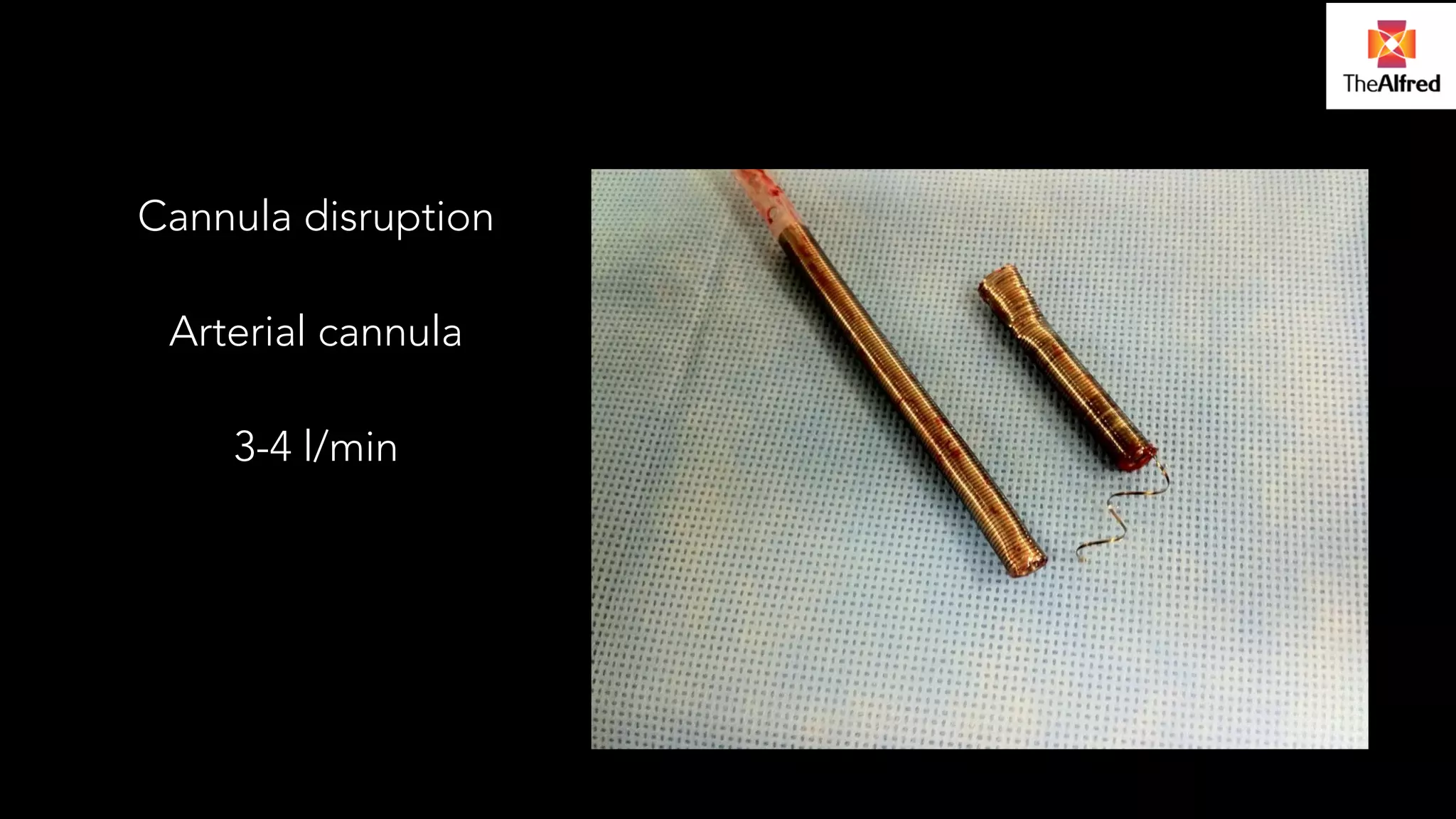
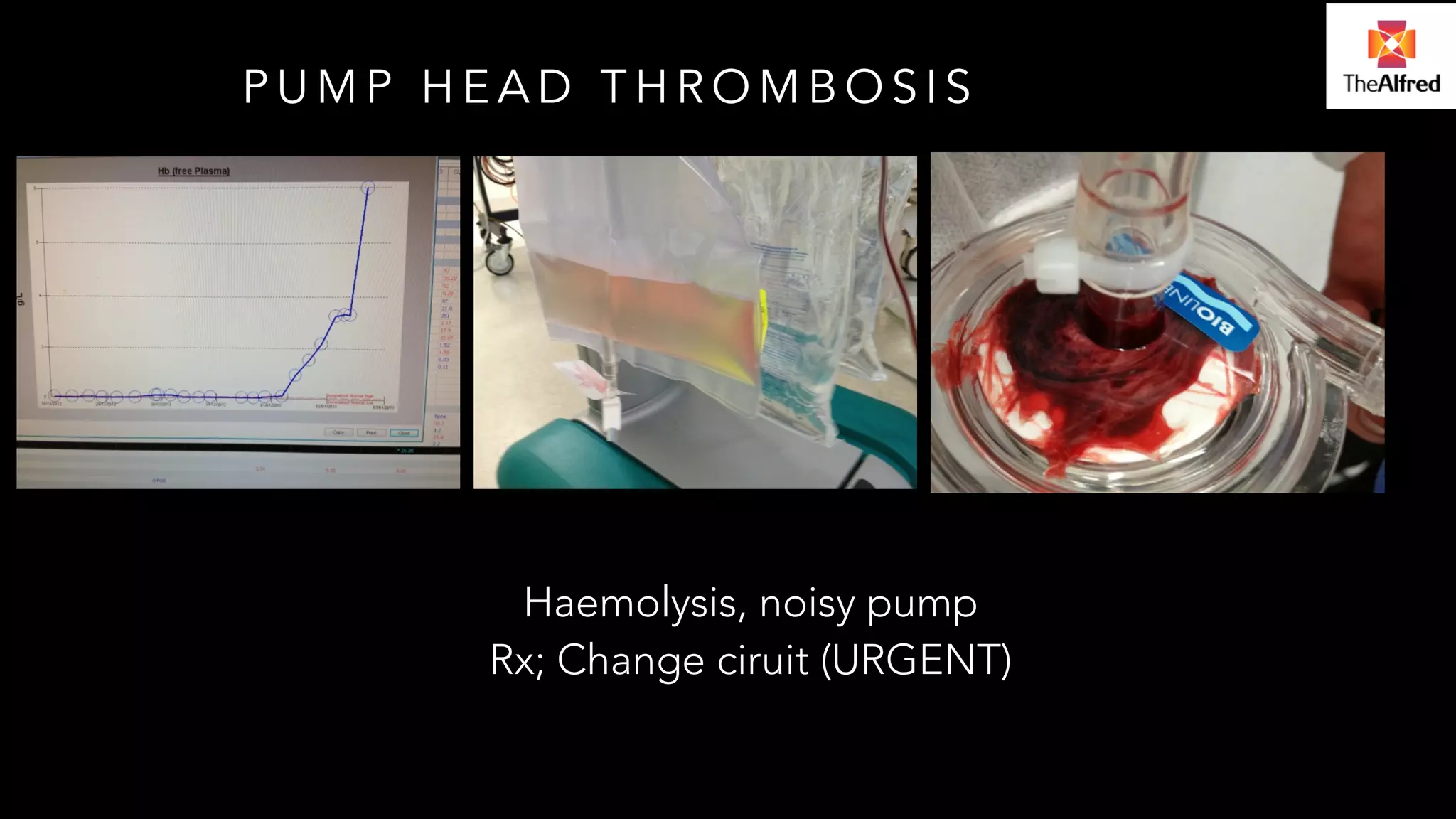
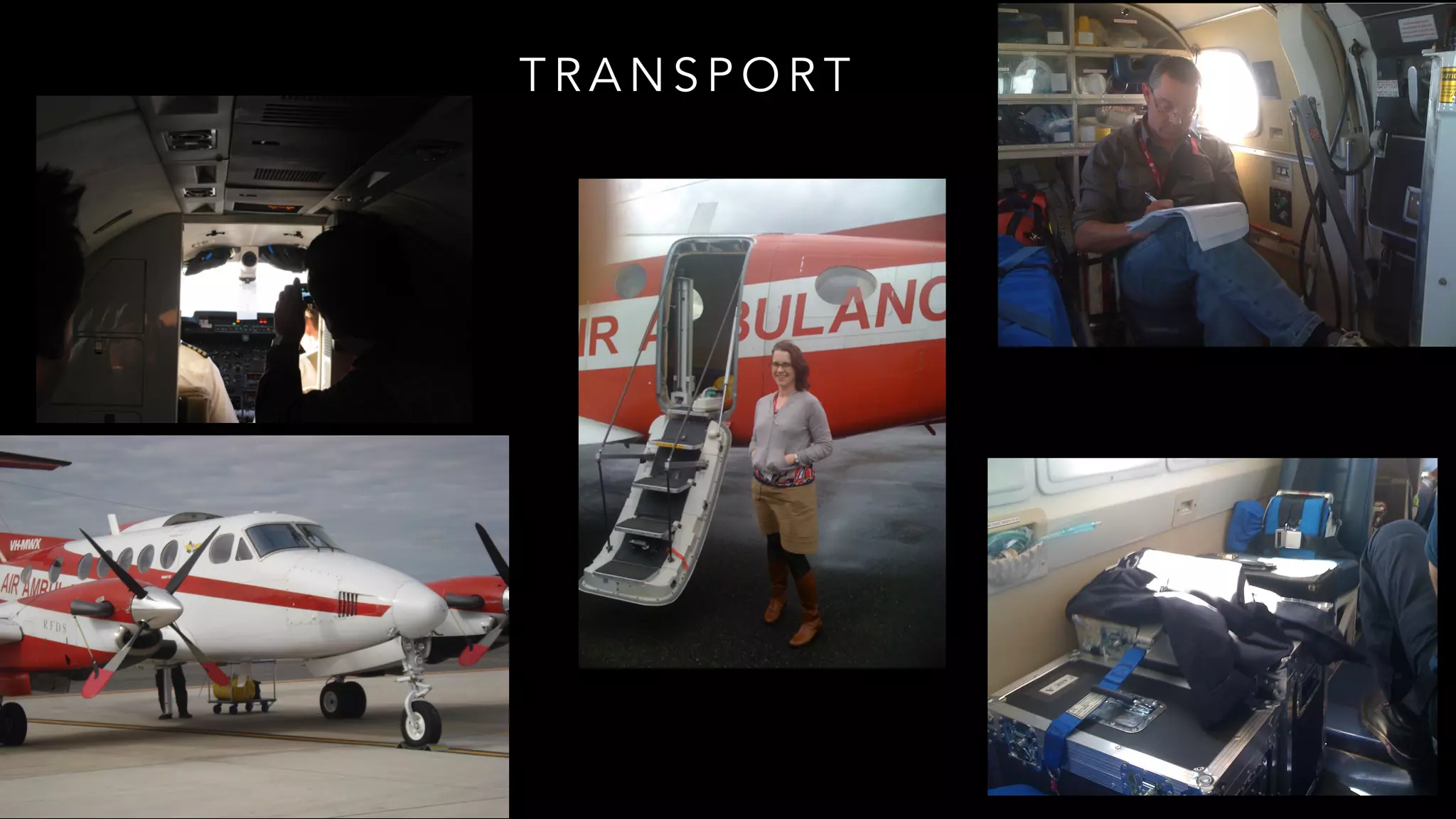
The document discusses the complexities and challenges associated with ECMO (extracorporeal membrane oxygenation), emphasizing the importance of proper patient selection, cannulation techniques, and maintenance to avoid complications. It outlines potential pitfalls during the initiation and maintenance phases, including vascular access issues, circuit complications, and the necessity for thorough training and simulation for healthcare teams. Additionally, the document stresses the importance of effective communication and knowledge sharing to enhance decision-making and minimize risks in high-stakes scenarios.