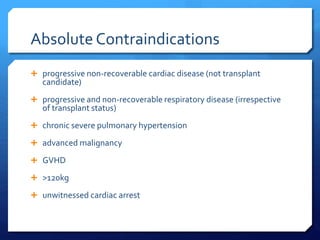
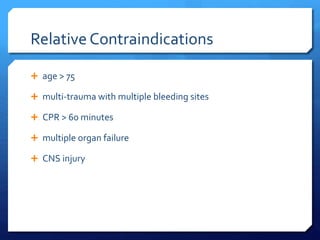
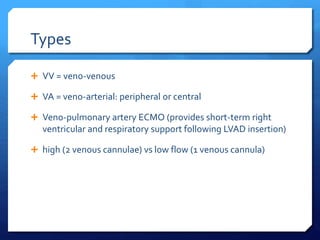
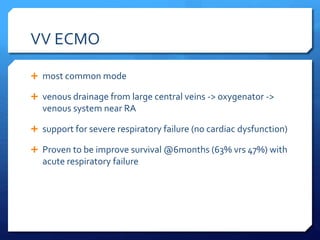
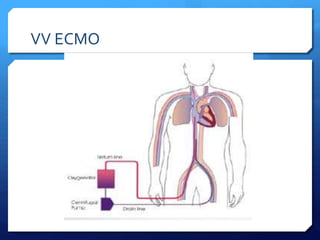
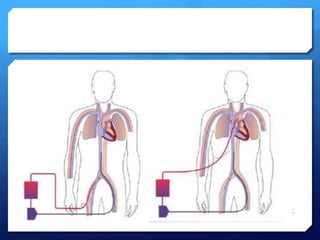
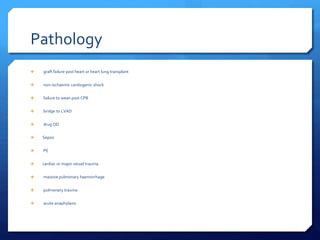
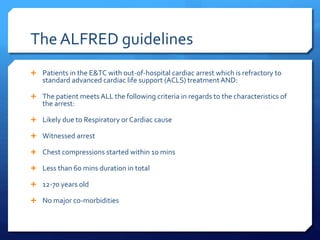
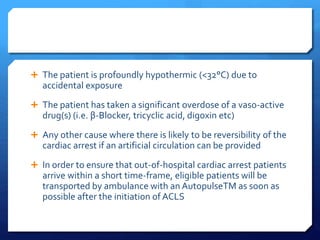
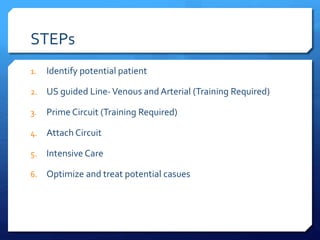
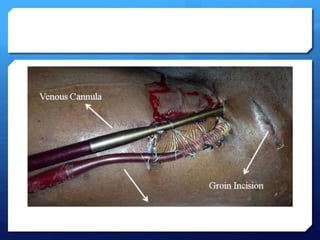
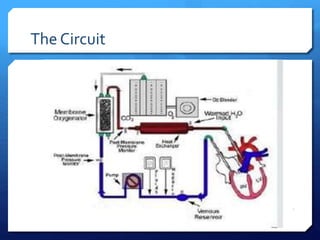
ECMO is a form of extracorporeal life support that oxygenates and removes carbon dioxide from the blood. It is being considered in the emergency department for patients experiencing refractory ventricular fibrillation during cardiac arrest. ECMO may improve survival rates and neurological outcomes compared to conventional CPR. There are indications and contraindications for its use in acute, severe reversible respiratory or cardiac failure. The two main types are veno-venous ECMO for respiratory failure and veno-arterial ECMO for cardiac failure. Proper patient selection, cannulation technique, and circuit management are important considerations for ECMO in cardiac arrest.