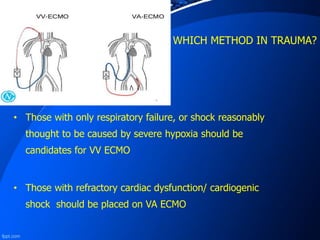
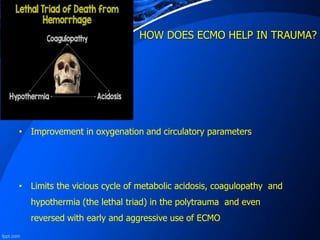
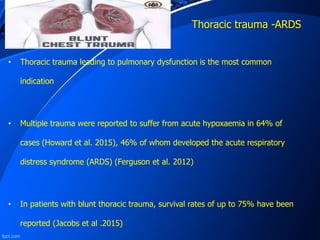
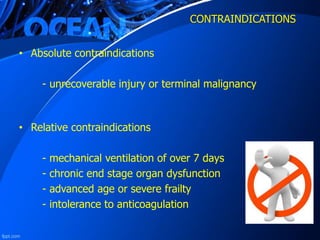
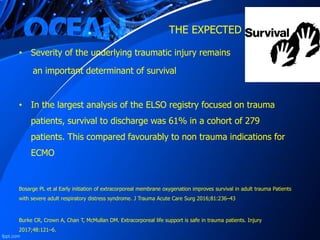
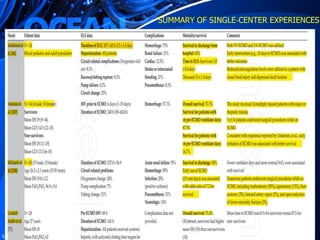
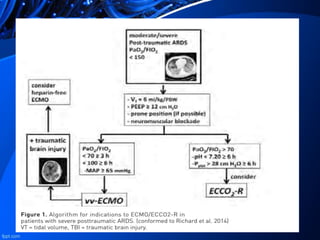
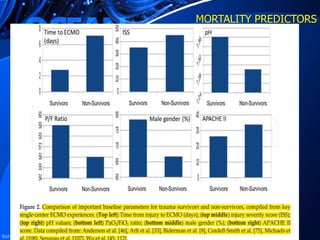
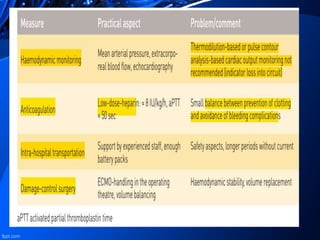
ECMO can be considered for partial or full cardiopulmonary support in cases of potentially reversible post-traumatic cardiopulmonary failure. Those with respiratory failure should be candidates for VV ECMO, while those with refractory cardiac dysfunction should receive VA ECMO. ECMO can improve oxygenation and circulation to limit complications like metabolic acidosis. Indications include severe lung injury from trauma leading to ARDS. Contraindications include unrecoverable injury or advanced organ dysfunction. While outcomes are best at high-volume centers, ECMO may allow time for injury recovery or organ donation in severe trauma.