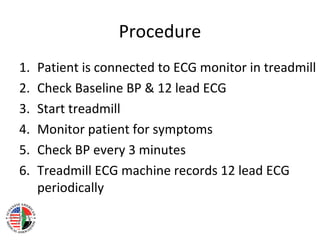
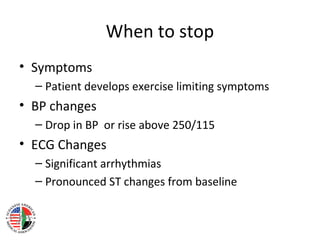
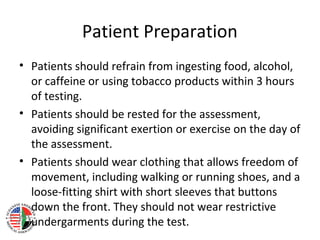
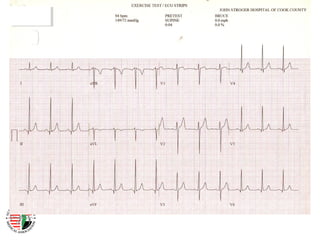
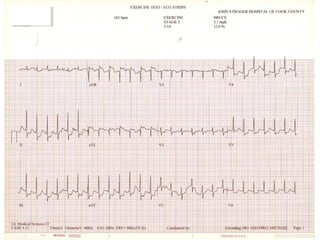
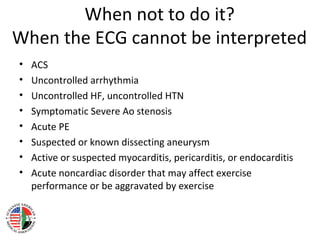
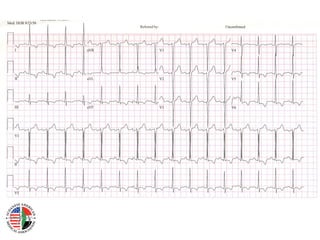
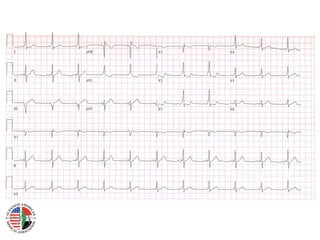
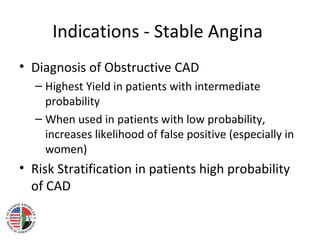
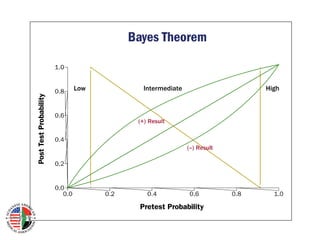
This document provides information about exercise electrocardiogram (ECG) stress testing for internists. It discusses the principles, purpose, procedures, patient preparation, understanding the report, contraindications, and indications for stress testing. The main points are: stress testing elicits cardiovascular abnormalities not seen at rest and determines cardiac function; it estimates prognosis and likelihood of coronary artery disease; procedures involve monitoring ECG and symptoms during treadmill exercise; the report details exercise duration, heart rate changes, symptoms, and any ECG abnormalities; contraindications include recent acute cardiac issues or inability to interpret ECG; and indications include diagnosing stable angina and risk stratifying unstable angina or recent heart attacks.