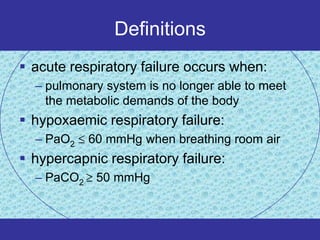
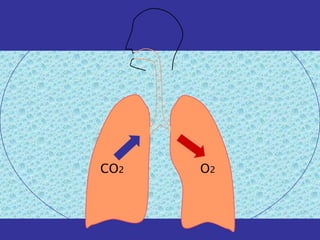
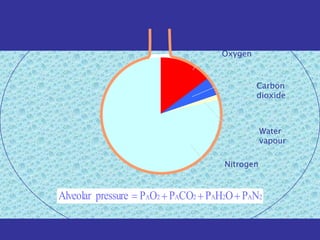
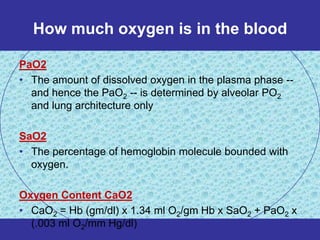
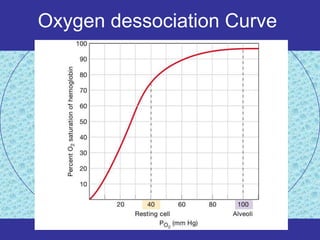
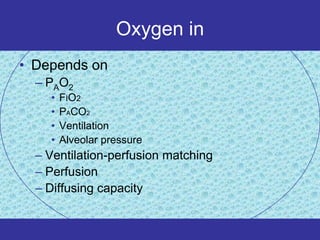
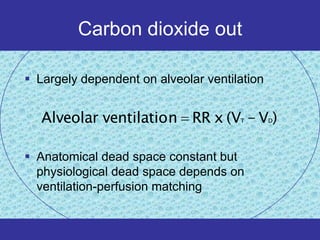
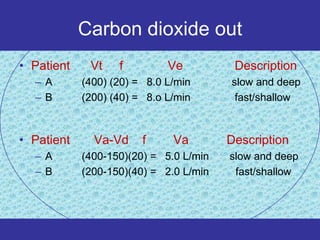
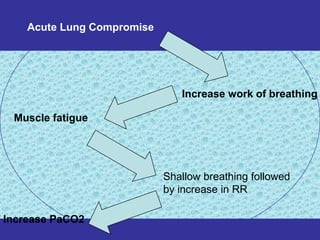
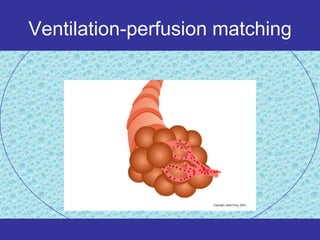
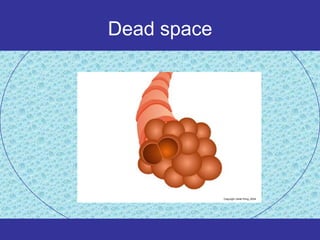
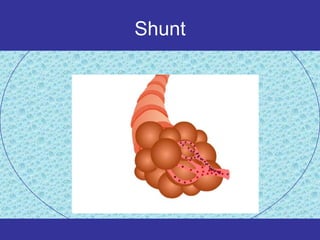
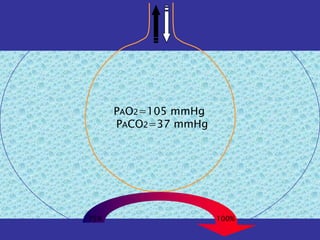
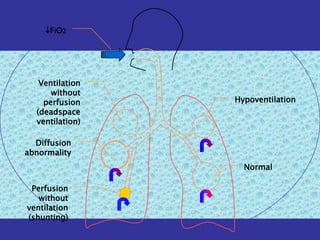
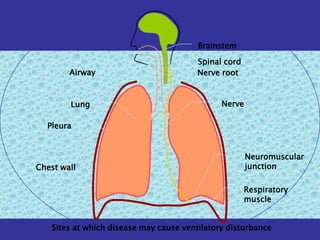
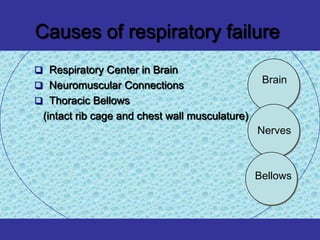
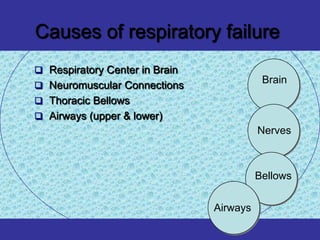
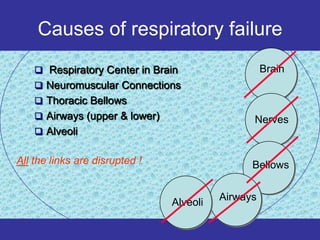
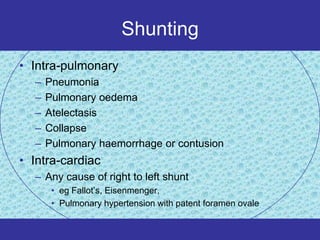
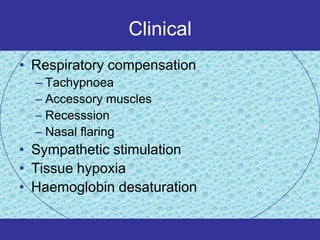
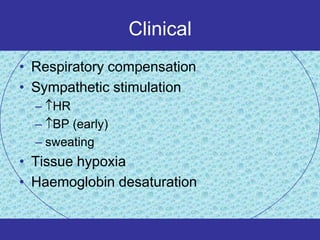
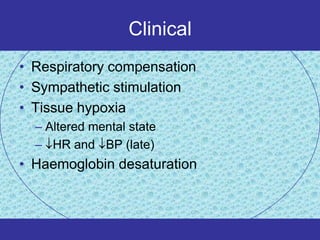
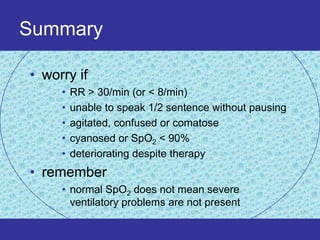
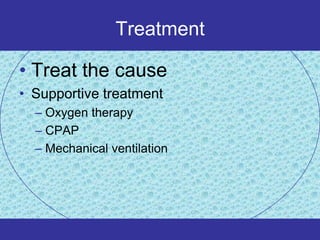
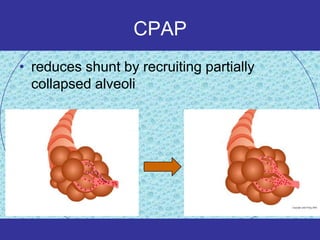
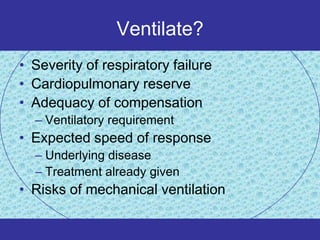
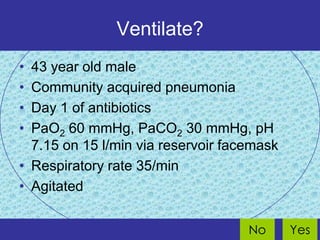
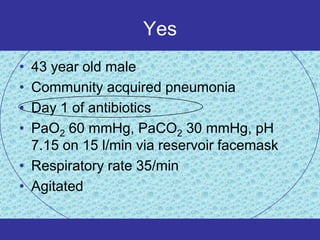
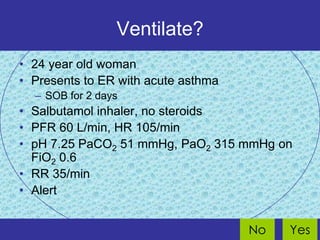
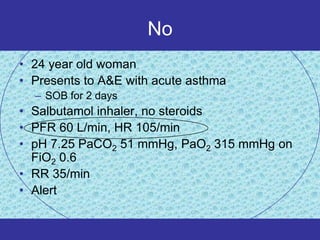
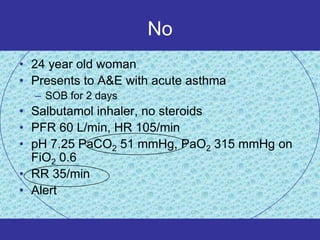
Acute respiratory failure occurs when the pulmonary system can no longer meet the body's metabolic demands. It can be hypoxaemic, with an oxygen level below 60 mmHg, or hypercapnic, with a carbon dioxide level over 50 mmHg. Respiratory failure results from issues in oxygen intake and carbon dioxide removal, due to problems in ventilation, perfusion matching, gas exchange, or other pathologies. It is monitored clinically and with blood tests, and treated by addressing the underlying cause, providing supportive oxygen therapy or ventilation support like CPAP or mechanical ventilation if needed.