Title page
Objectives
Outlines of the presentation
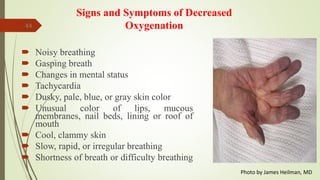
Introduction about schizophrenia types and signs and symptoms
Nursing diagnoses and behaviors commonly associated with psychotic disorders (Table 3-24)
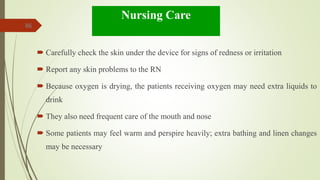
Nursing diagnoses for patients with schizophrenia, expected outcomes, and nursing interventions
Summary slide
References slide