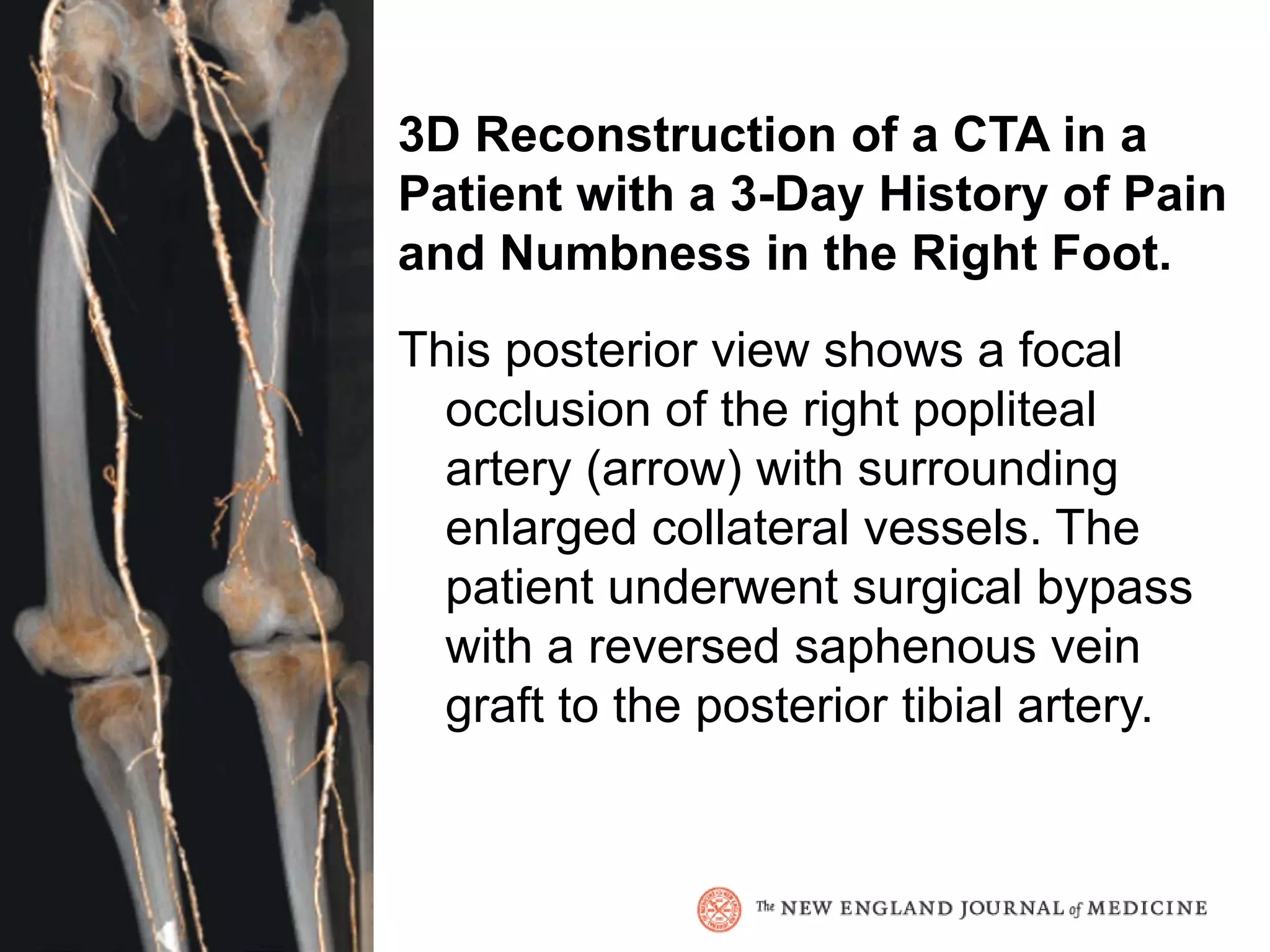
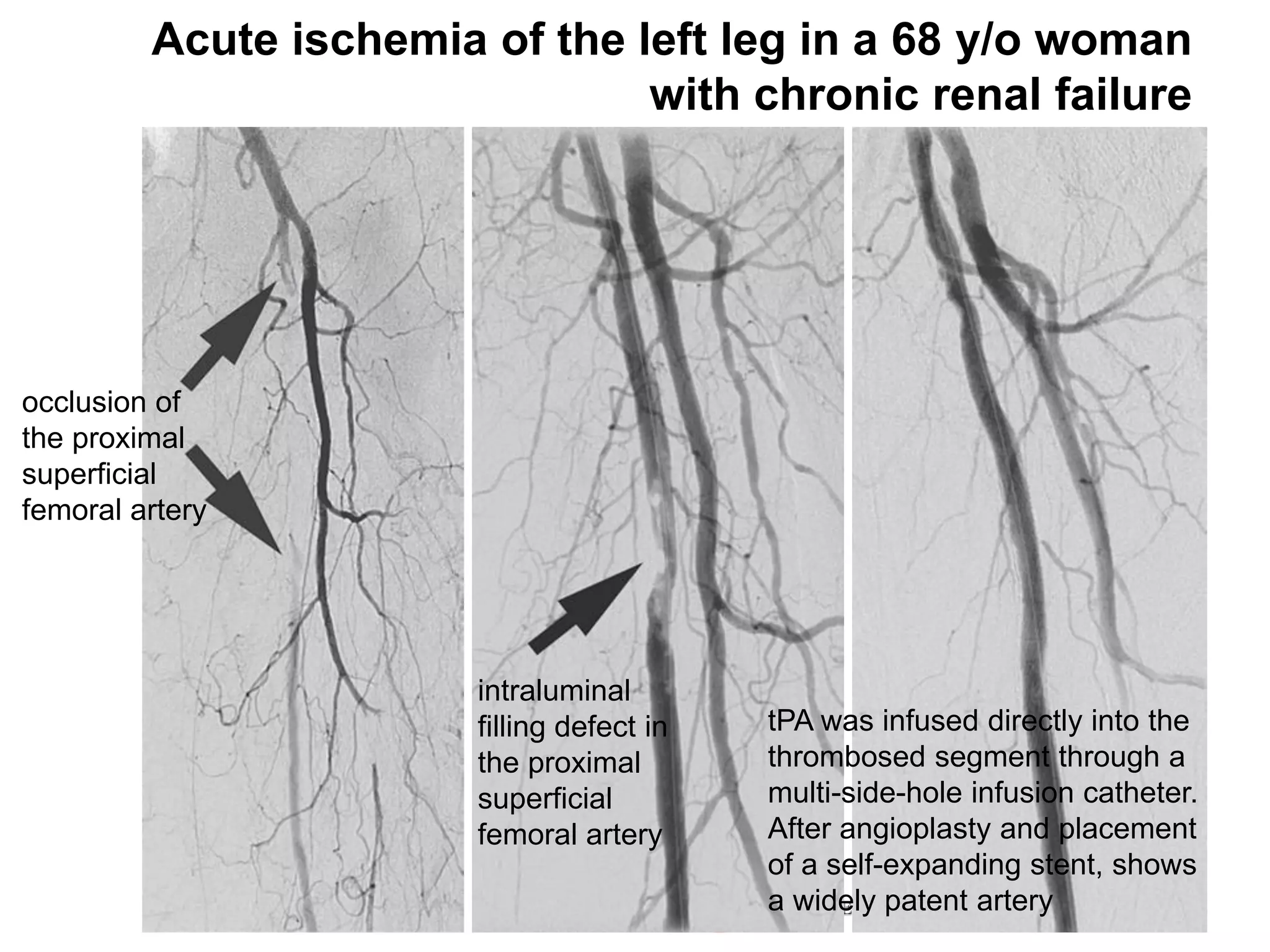
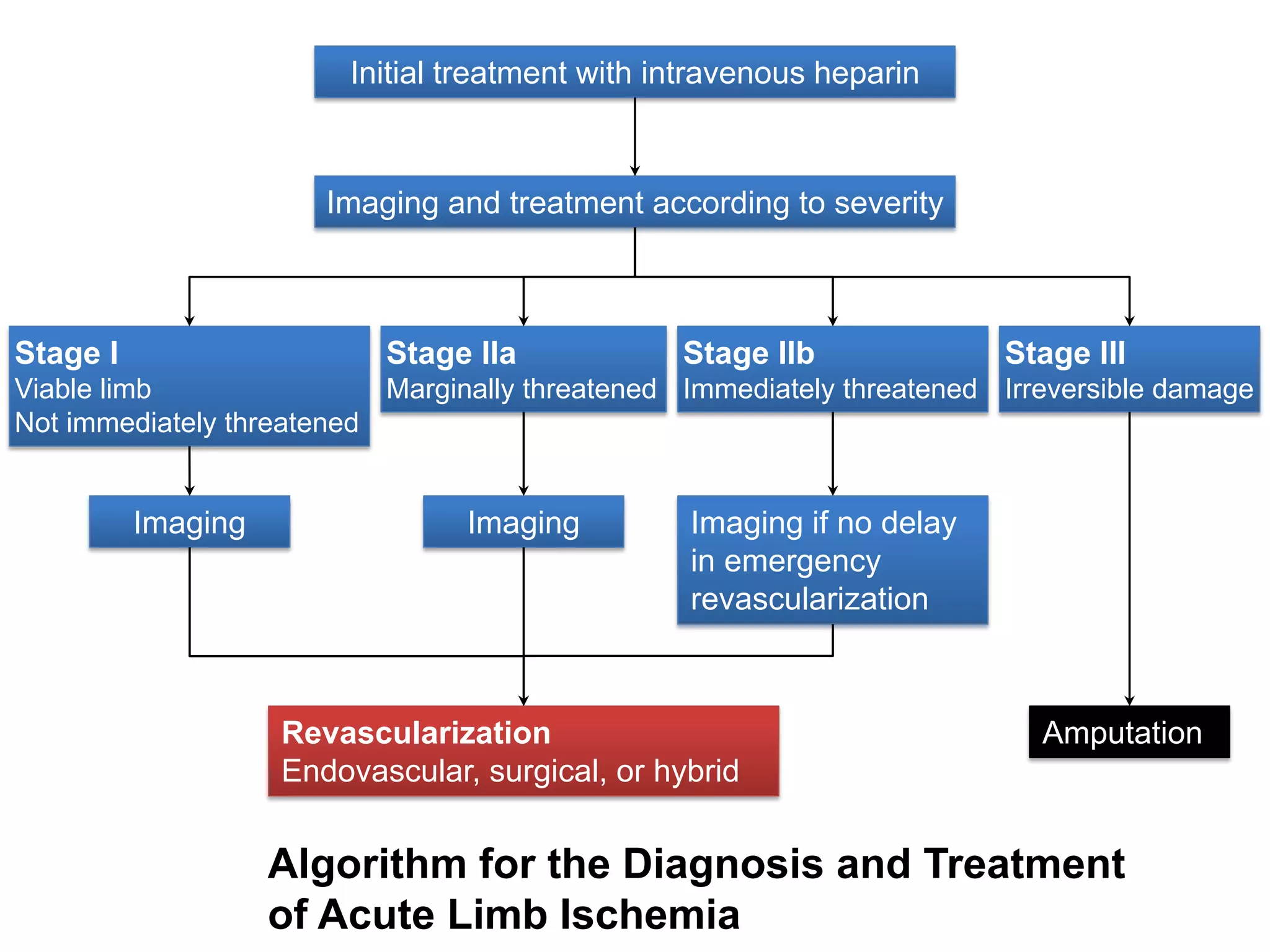
Acute limb ischemia is a sudden decrease in blood flow to a limb that threatens viability. It requires urgent evaluation and management to determine if the limb is viable, threatened, or irreversibly damaged. Prompt diagnosis and revascularization through catheter-based thrombolysis, thrombectomy, or surgery can reduce limb loss risk. Treatment approaches depend on the severity of ischemia and limb threat.