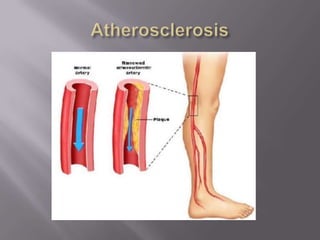
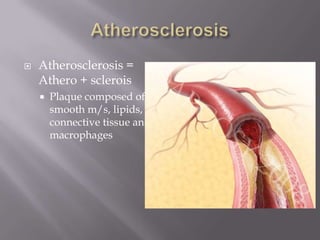
1. The document discusses peripheral arterial occlusive disease (PAOD), also known as peripheral artery disease (PAD), which refers to obstruction of arteries outside the heart and brain.
2. Risk factors for PAOD include smoking, diabetes, hypertension, hyperlipidemia, older age, male sex, family history of vascular disease, and certain ethnicities.
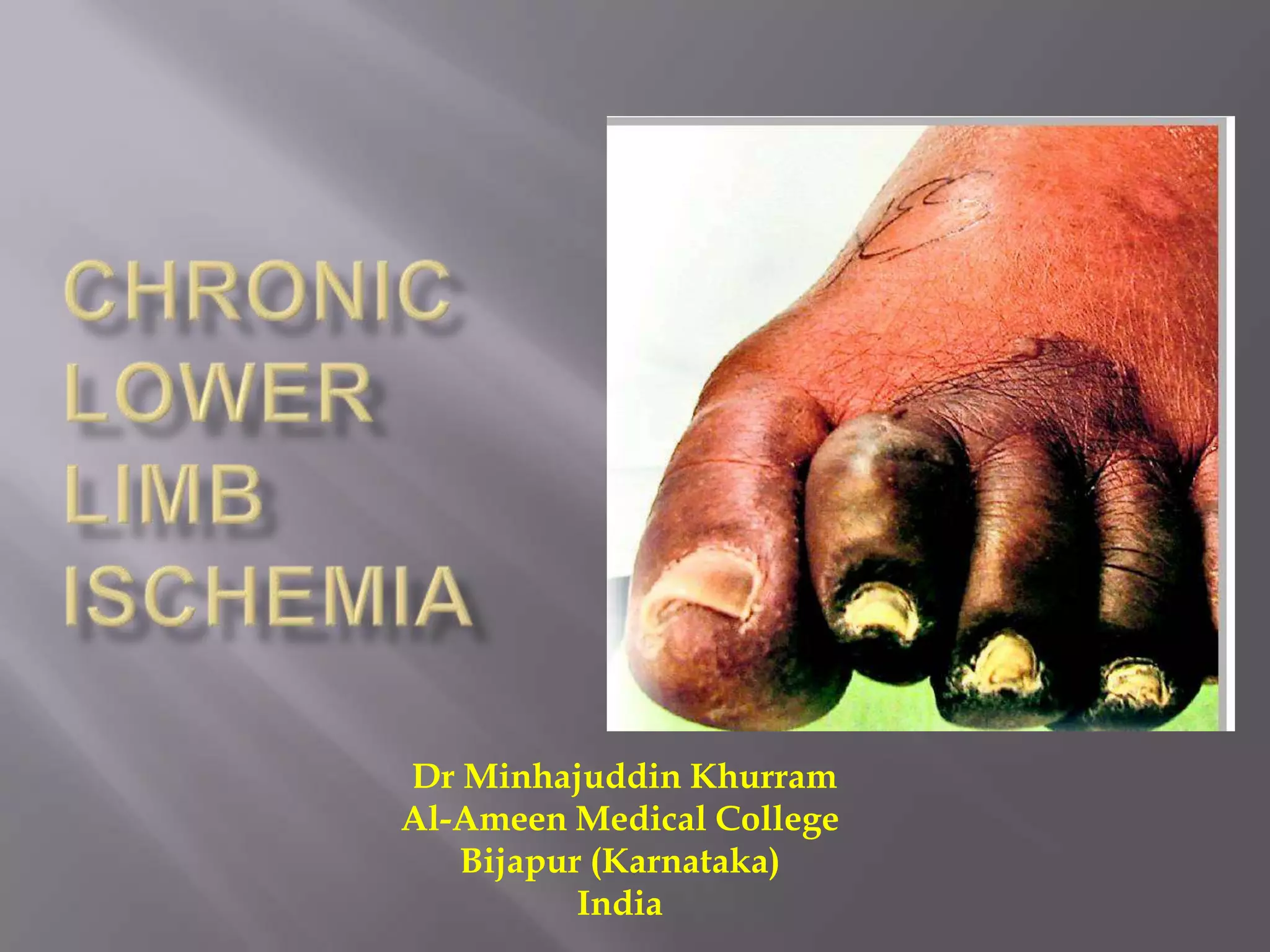
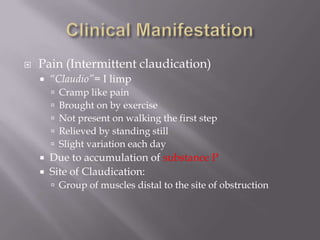
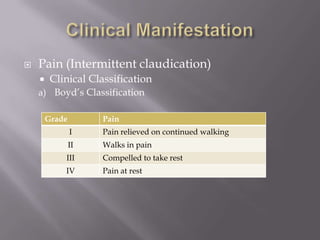
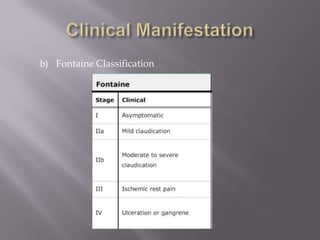
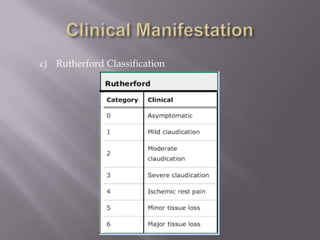
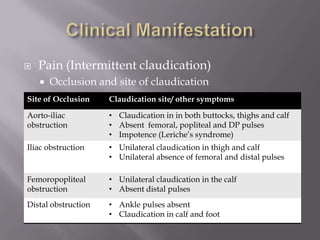
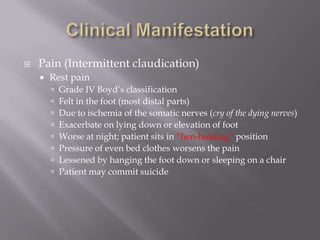
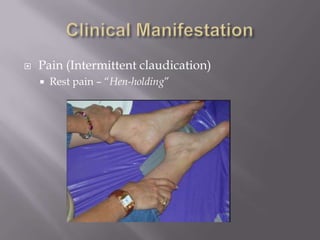
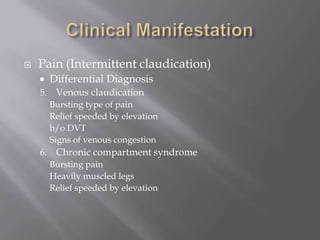
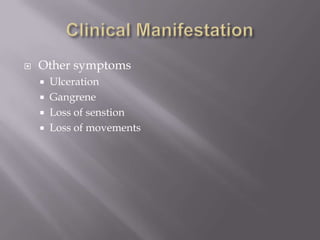
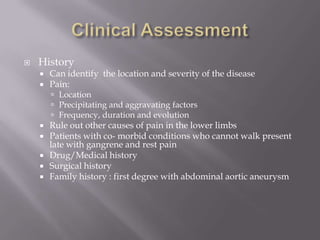
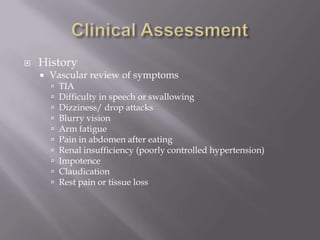
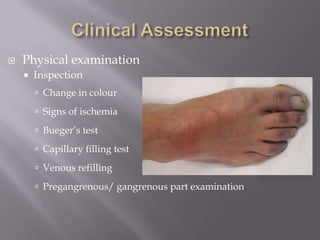
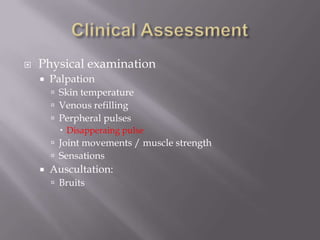
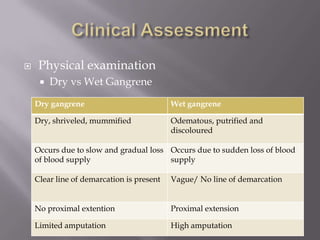
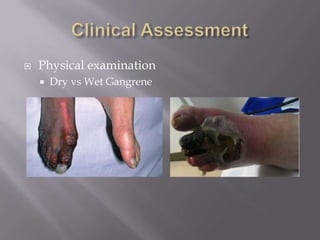
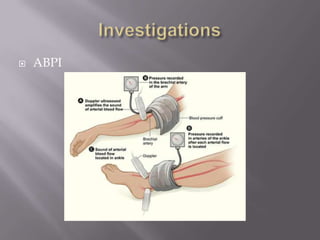
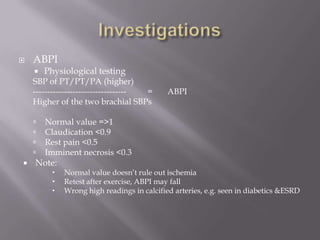
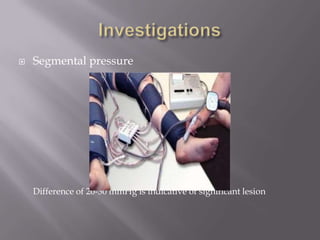
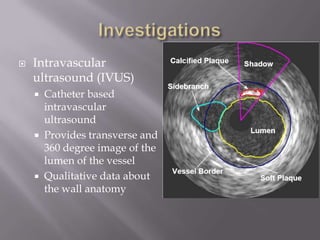
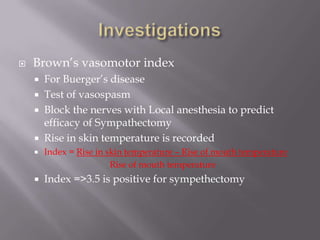
3. Symptoms range from intermittent claudication to critical limb ischemia with rest pain and tissue loss. Physical exam findings and tests like the ankle-brachial pressure index can help in diagnosis.
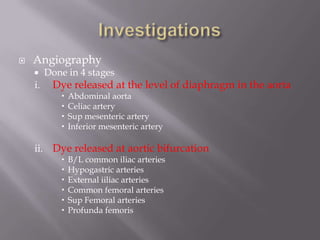
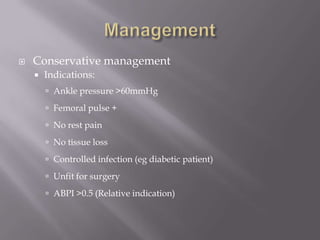
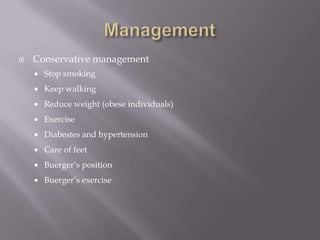
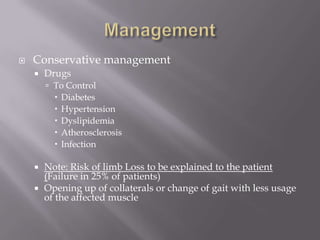
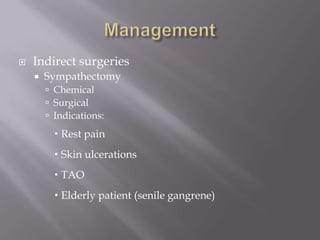
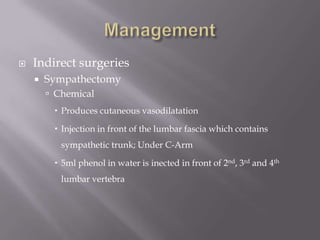
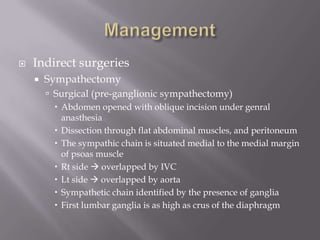
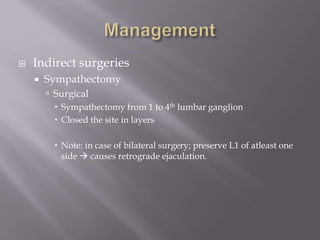
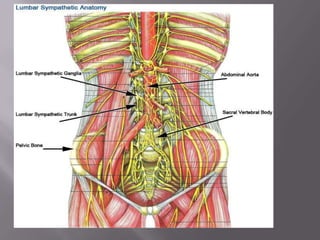
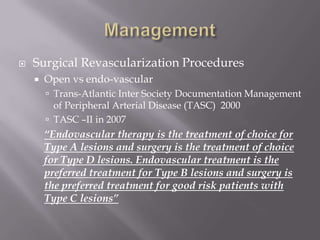
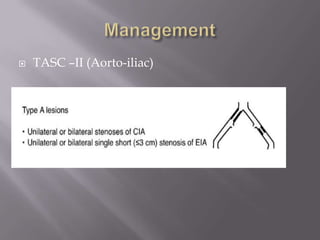
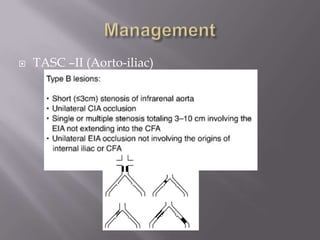
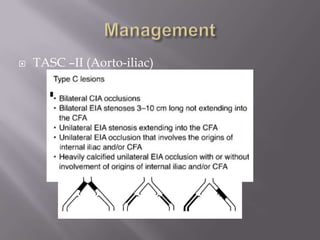
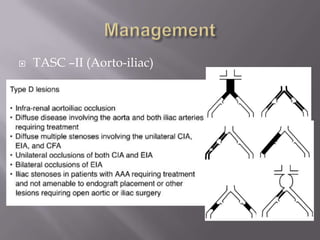
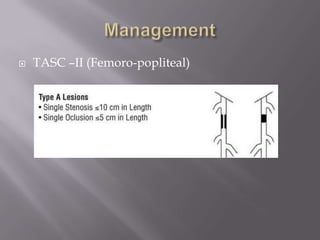
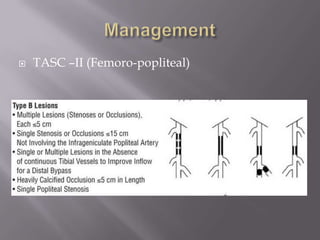
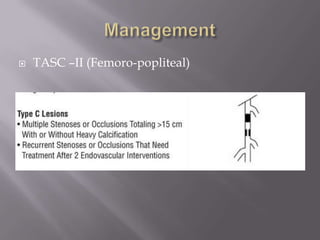
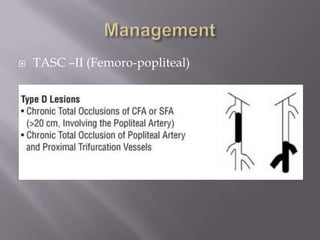
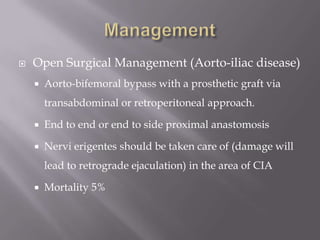
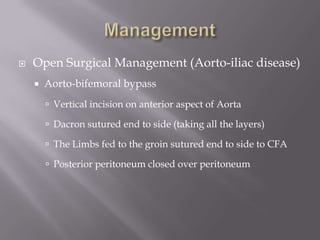
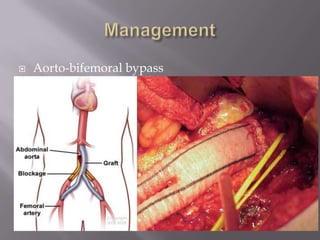
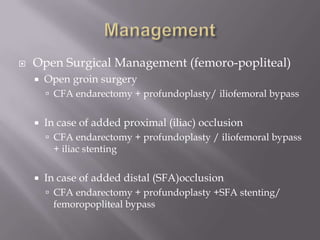
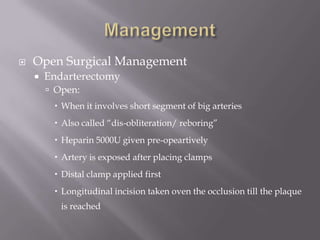
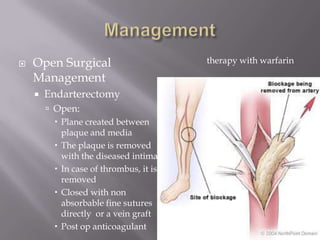
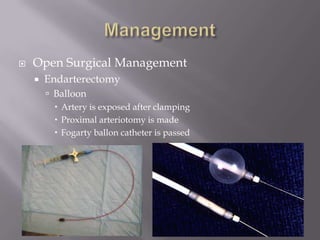
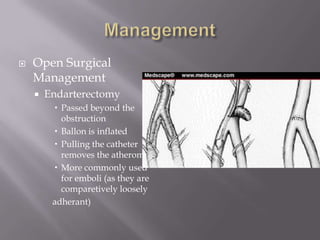
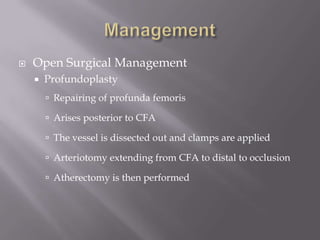
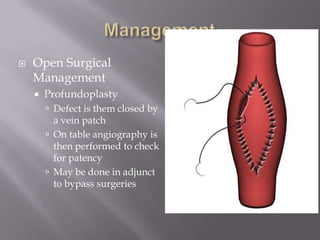
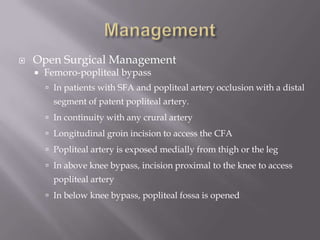
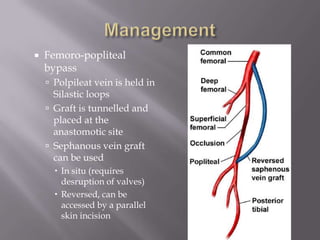
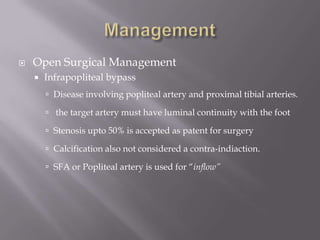
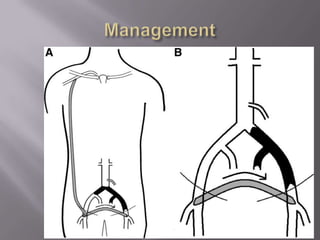
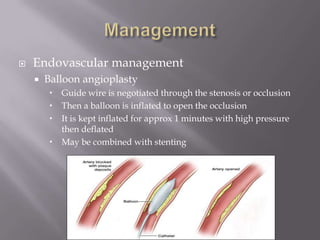
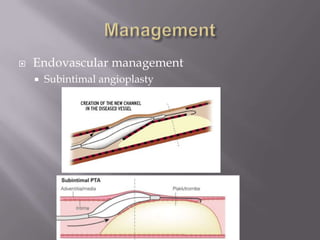
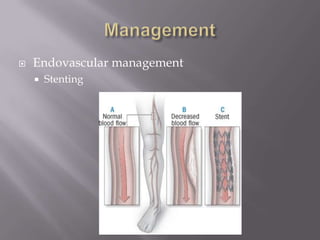
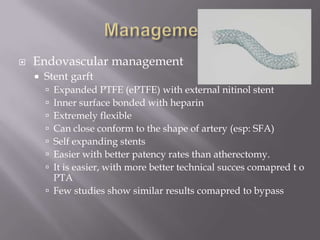
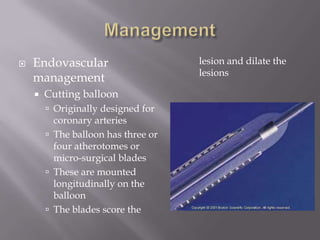
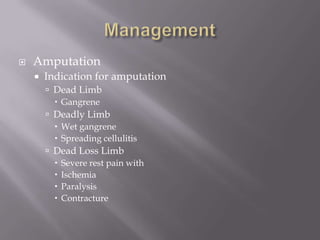
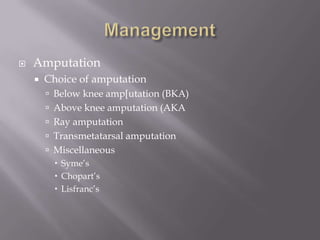
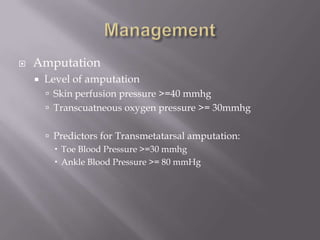
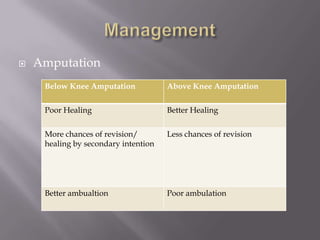
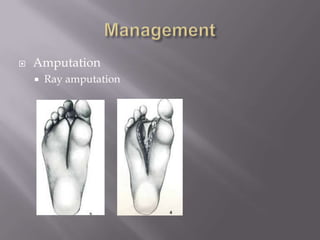
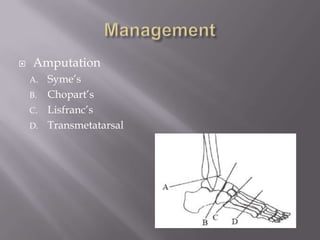
4. Management options discussed include conservative treatment for mild cases as well as endovascular and surgical revascularization procedures for more severe cases.