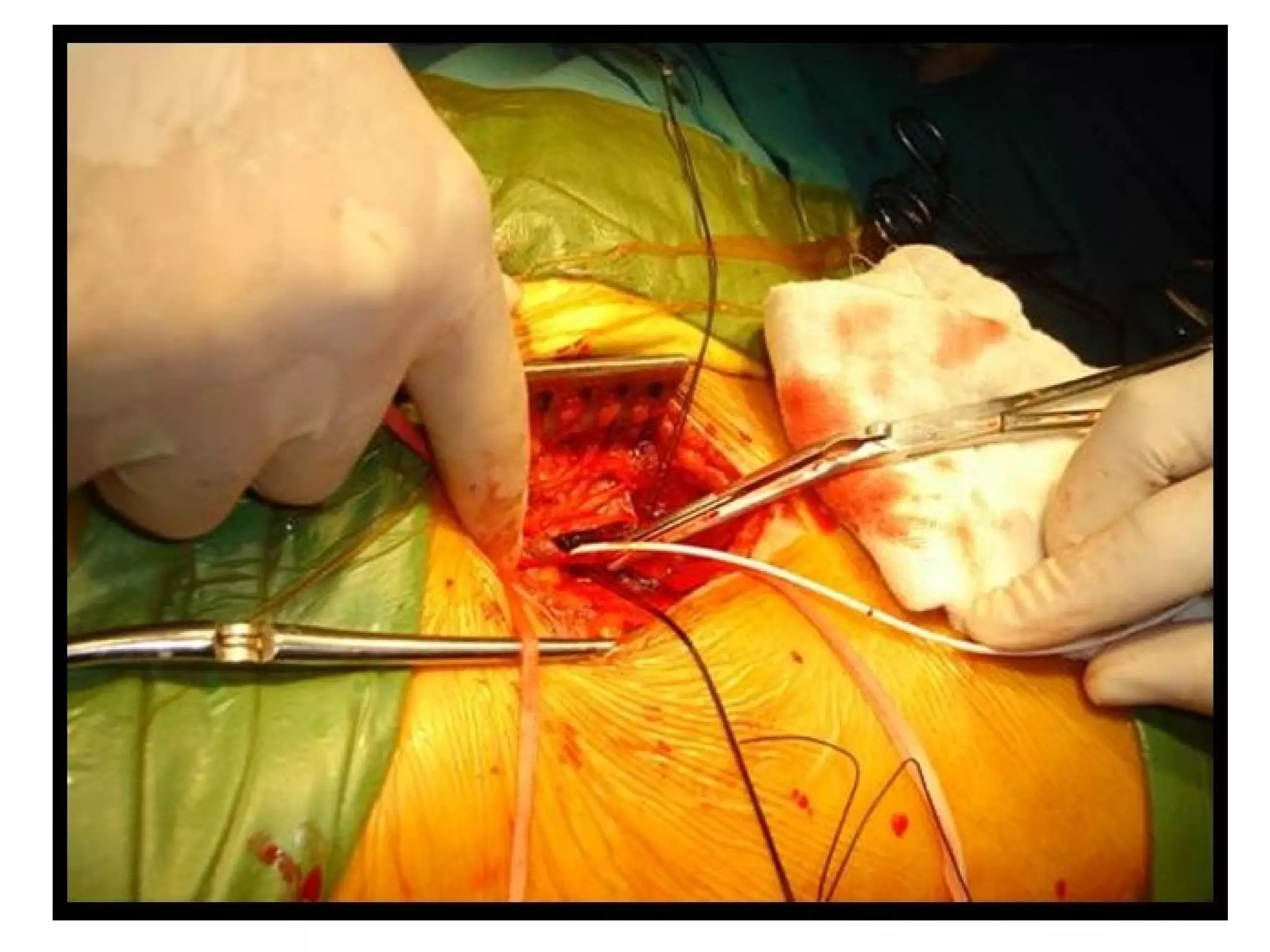
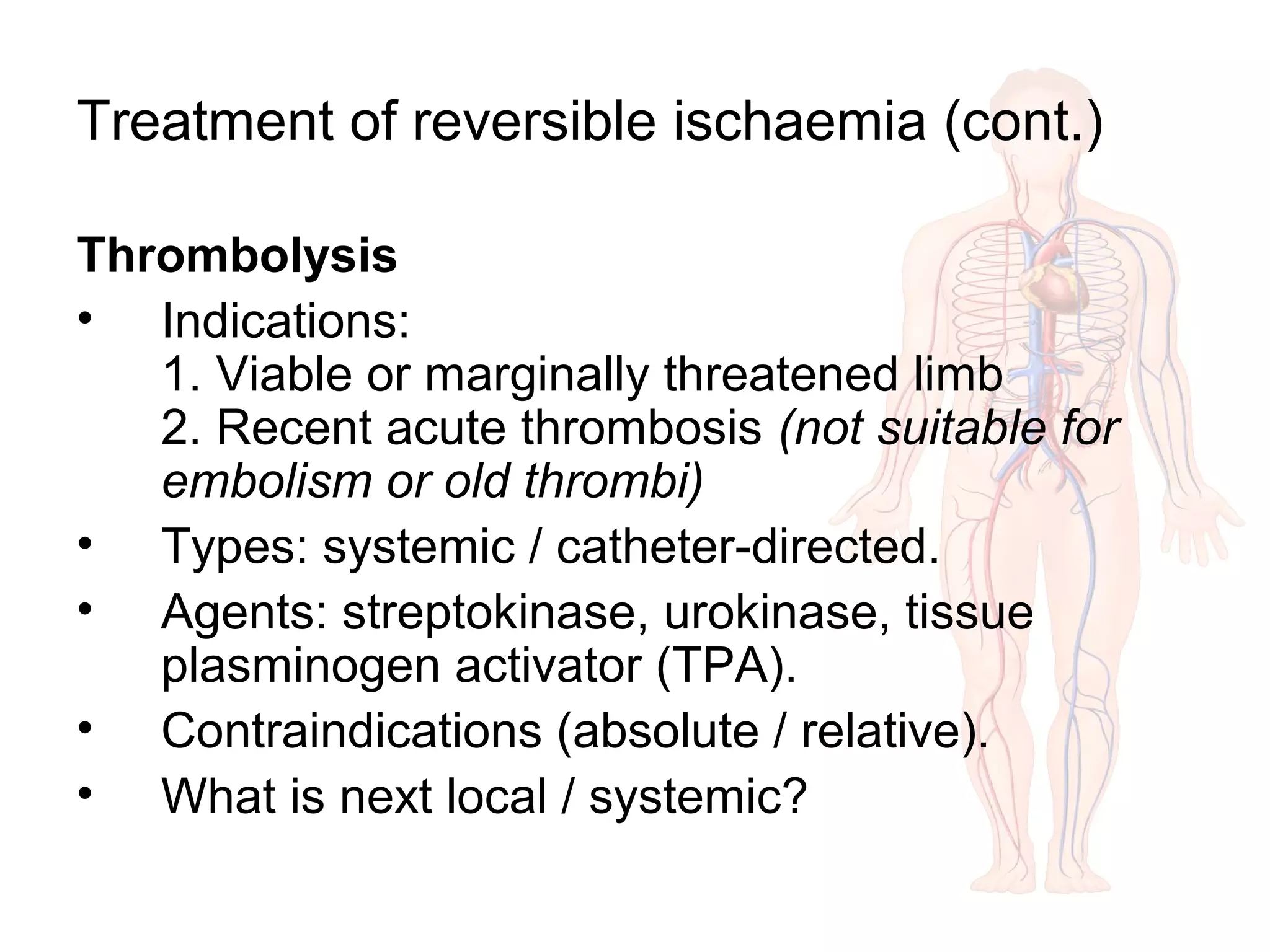
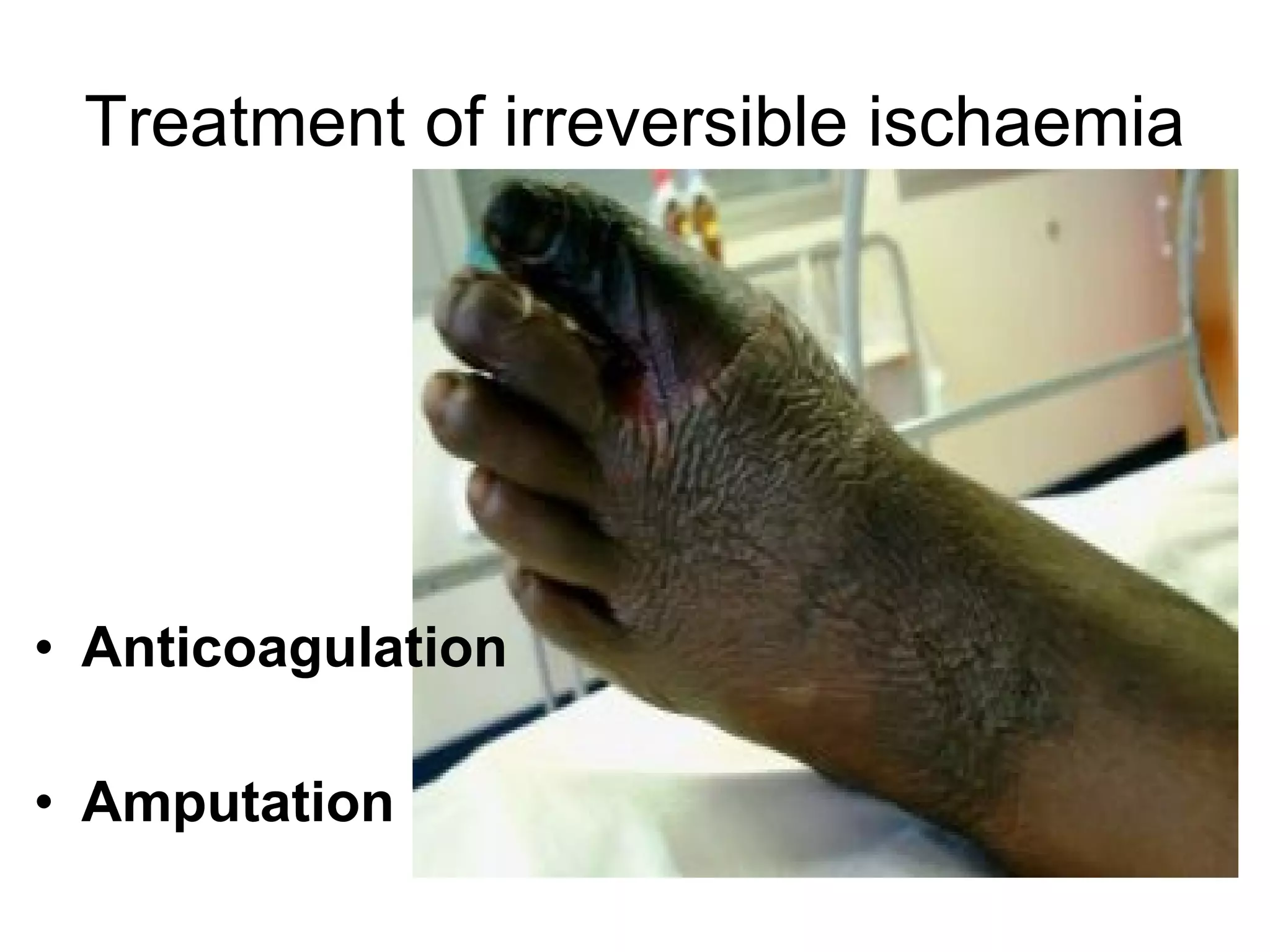
Acute limb ischemia is a sudden interruption of blood flow to a limb that requires prompt diagnosis and treatment to prevent tissue death. It is commonly caused by arterial embolism or thrombosis. Clinical signs include the six Ps: pain, pallor, paresthesia, pulselessness, poikilothermia, and paralysis. Diagnosis involves Doppler ultrasound, angiography, and investigating for potential causes such as cardiac problems. For reversible ischemia, treatment involves anticoagulation, thrombolysis, or surgical embolectomy/thrombectomy. Irreversible ischemia requires amputation to prevent limb and life-threatening complications. Prompt diagnosis and treatment of the underlying cause are crucial to limb salvage.