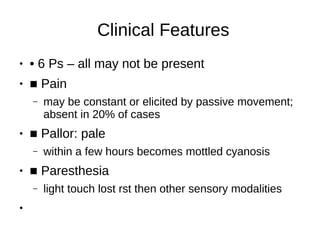
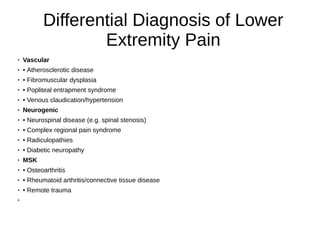
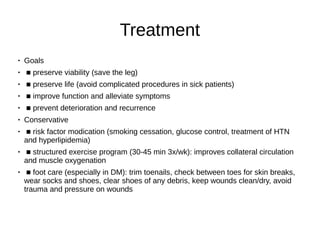
This document discusses vascular surgery, specifically acute arterial ischemia and chronic limb ischemia/peripheral artery disease (PAD). For acute arterial ischemia, urgent management is needed within 6 hours to prevent irreversible muscle damage. Etiologies include embolism and thrombosis. Clinical features include the 6 Ps. Investigations and treatment involve angiography, embolectomy, thrombectomy or bypass grafting. Chronic limb ischemia/PAD is usually due to atherosclerosis and presents with claudication or critical limb ischemia. Treatment involves risk factor modification, exercise, pharmacotherapy such as statins, and surgical revascularization if conservative measures fail.















![Pharmacotherapy
● Patients with PAD are at increased risk for CAD and CVD
●
■ antiplatelet agents (e.g. aspirin, clopidogrel)
● ■ statin
●
■ ACEI/ARB
● Surgical
●
■ Indications: severe lifestyle impairment, vocational impairment, critical ischemia
● ■ revascularization
●
◆ endovascular (angioplasty ± stenting)
● ◆ endarterectomy: removal of plaque and repair with patch (usually distal aorta or common/deep
femoral)
● ◆ bypass gra sites: aortofemoral, axillofemoral, femoropopliteal, femoro-tibial, femorofemoral bypass
●
◆ gra choices: saphenous vein graft (reversed or in situ), synthetic [polytetrauoroethylene gra (e.g.
Gore-Tex® or Dacron®)]
●
Amputation: if not anatomically suitable for revascularization, persistent serious infections/gangrene
unremitting rest pain that is poorly controlled with analgesics, medically unt for revascularization](https://image.slidesharecdn.com/vascularsurgery-220919150427-91712ebc/85/Vascular-Surgery-pdf-20-320.jpg)


