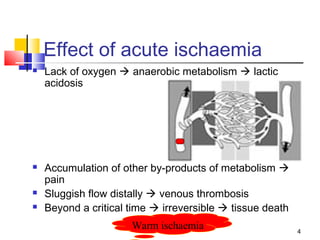
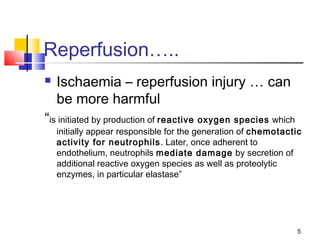
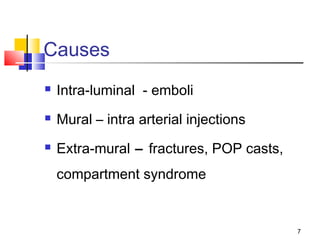
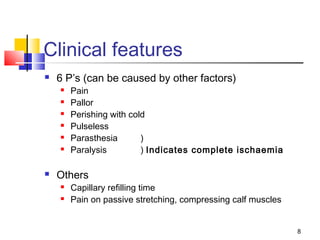
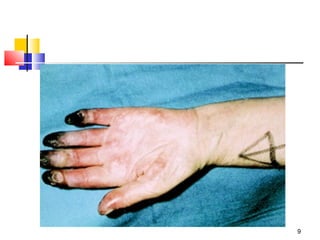
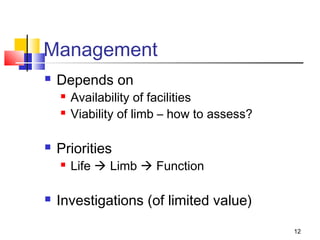
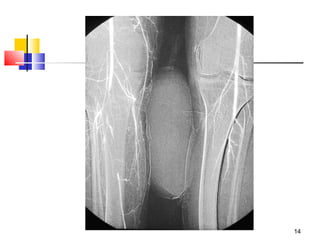
Acute limb ischaemia can be caused by emboli, injuries that damage blood vessels, or compression of the limb. This cuts off blood flow and oxygen to the tissues, leading to pain, discoloration, and eventual tissue death if not treated. Immediate management focuses on restoring blood flow through treatments like thrombolysis or surgery, while minimizing further tissue damage through measures like heparin and fasciotomy. The priority is saving life first, then limb, and ultimately function if possible.