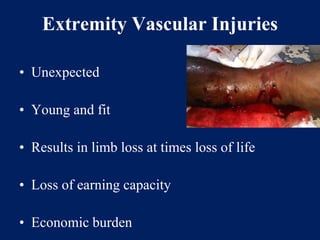
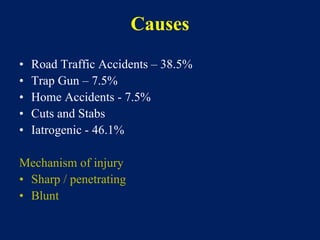
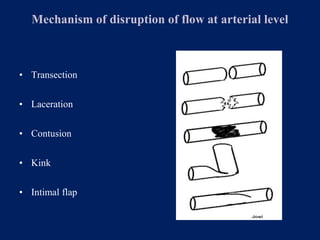
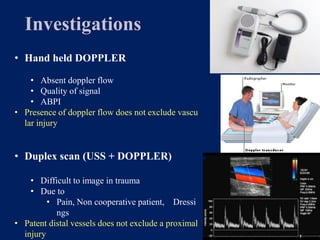
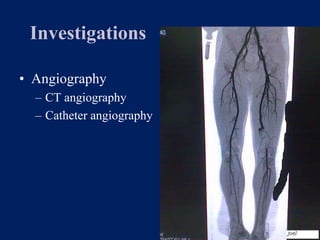
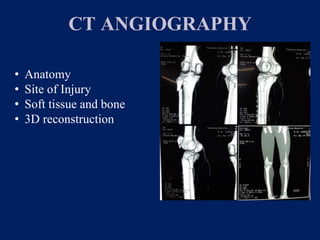
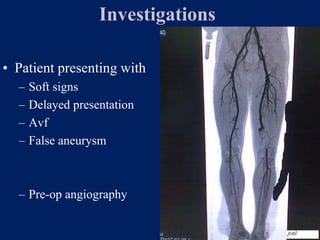
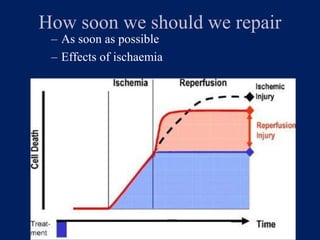
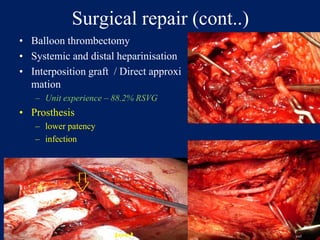
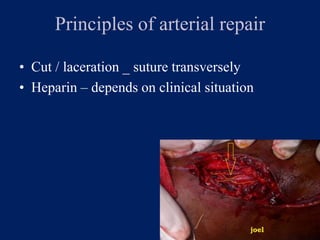
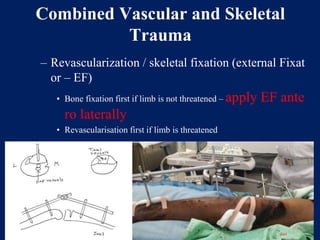
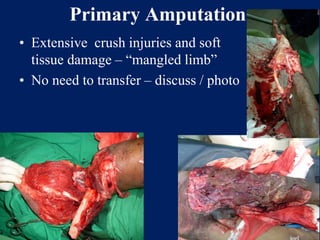
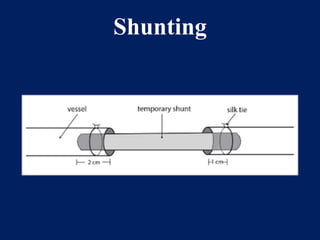
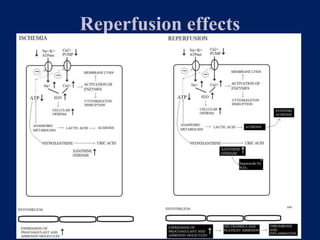
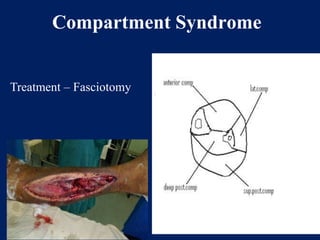
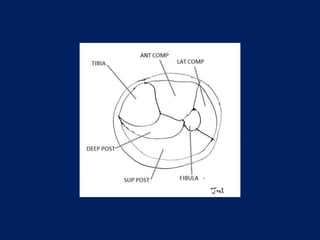
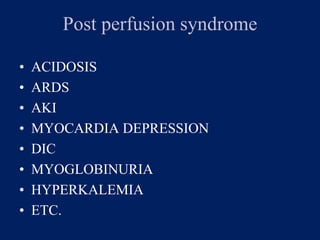
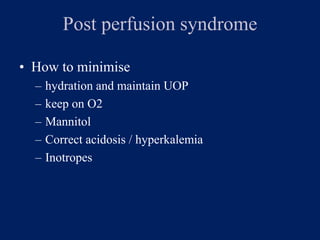
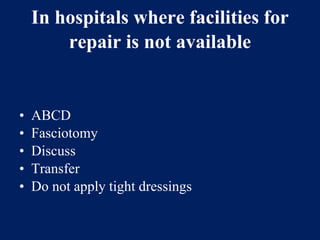
The document discusses vascular trauma, which includes injuries to arteries and veins in various anatomical regions such as extremities, abdomen, and thorax. It outlines causes, mechanisms of injury, signs of vascular injury, and the importance of timely diagnosis and surgical repair. The document emphasizes the management of vascular injuries, potential complications, and the need for urgent intervention to restore blood flow and limb viability.