The document discusses the acute abdomen and various imaging modalities used to evaluate it. It covers:
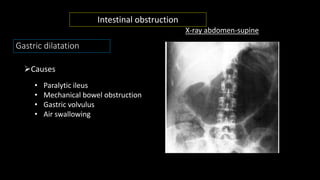
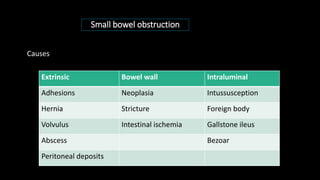
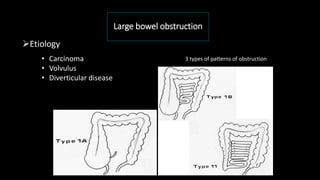
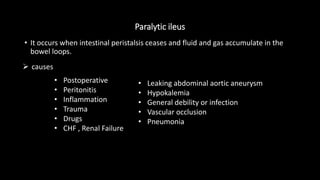
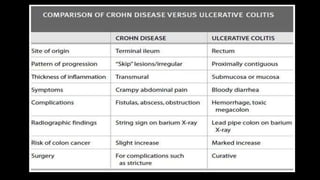
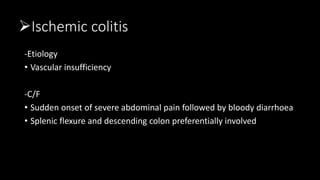
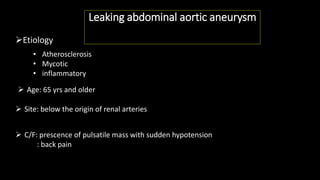
1) The causes of acute abdomen including perforation, obstruction, inflammation and others.
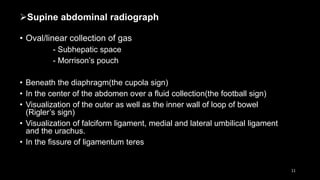
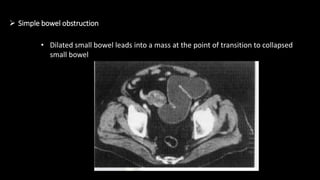
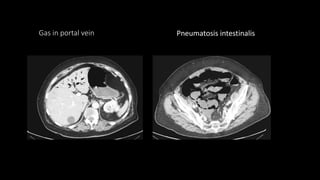
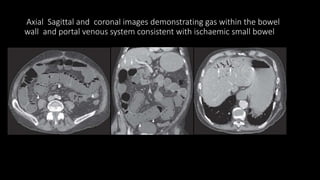
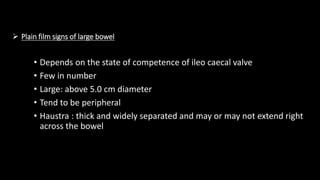
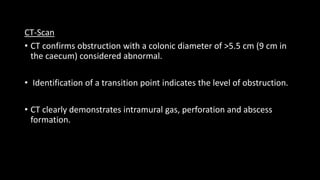
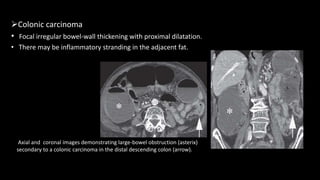
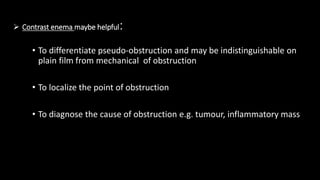
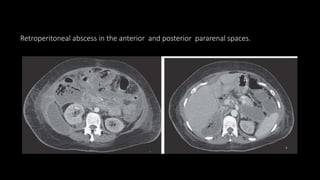
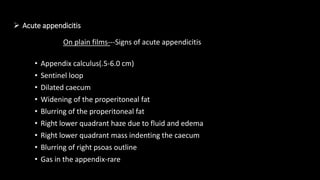
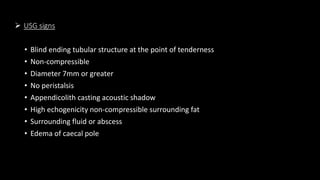
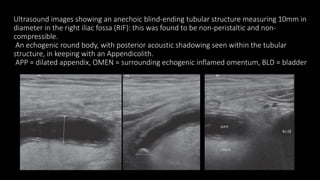
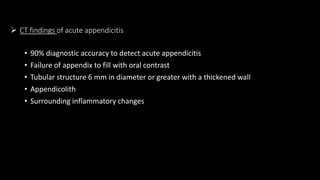
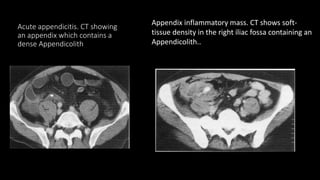
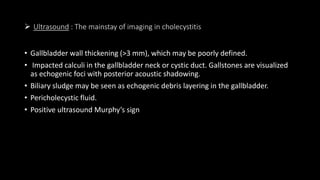
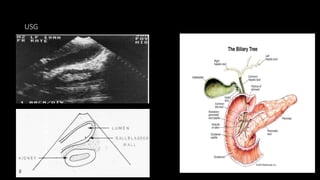
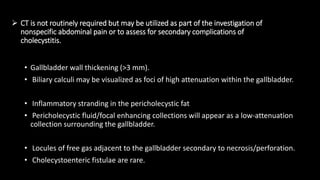
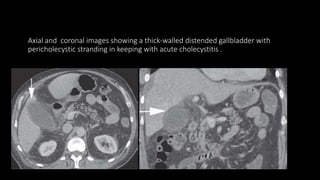
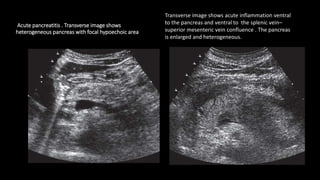
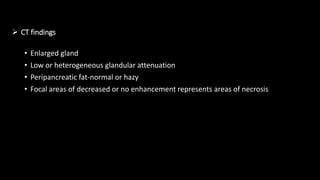
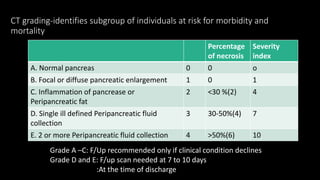
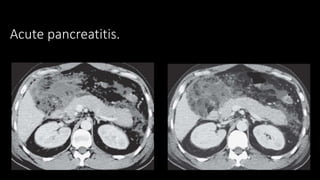
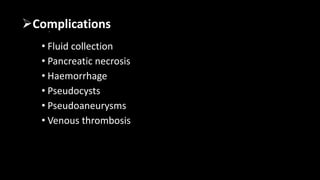
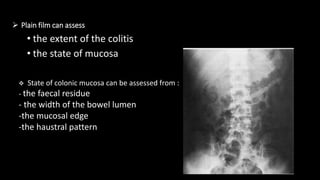
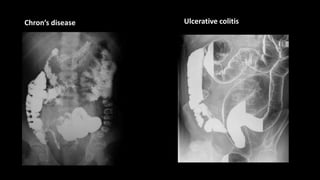
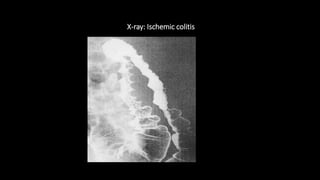
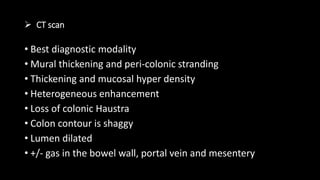
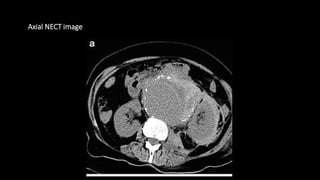
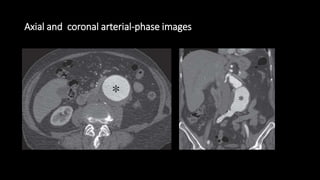
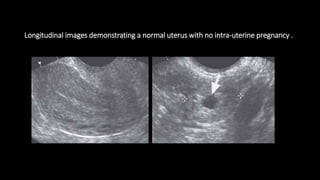
2) The imaging modalities used including plain films, ultrasound, CT and their roles in evaluating specific causes.
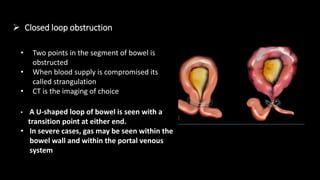
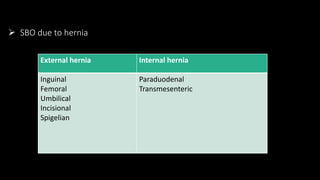
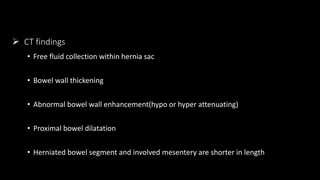
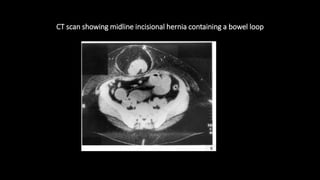
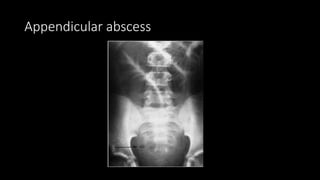
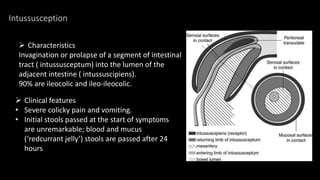
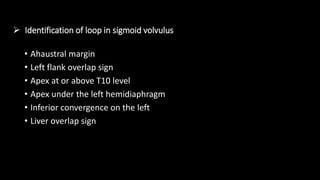
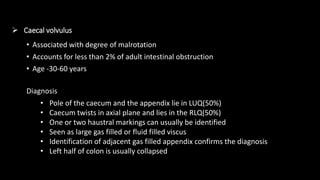
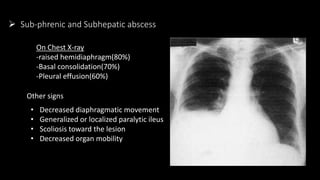
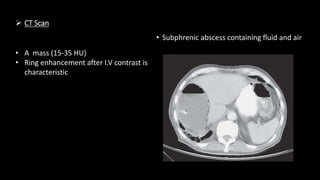
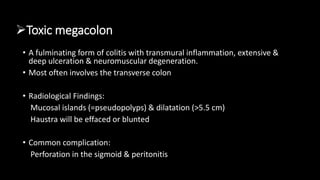
3) How different conditions present on imaging including bowel obstruction, perforation, appendicitis and others.