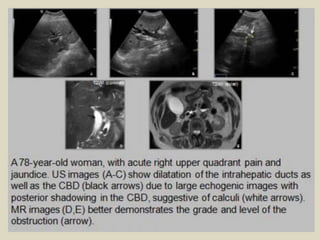
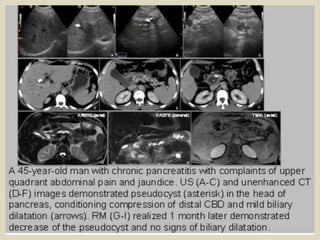
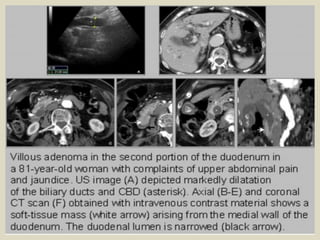
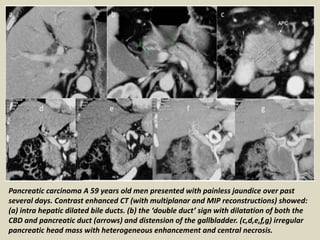
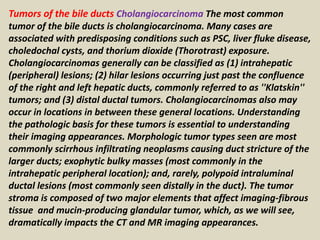
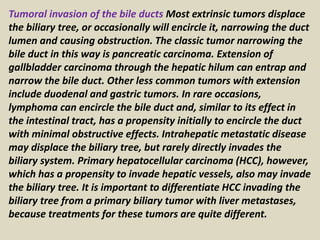
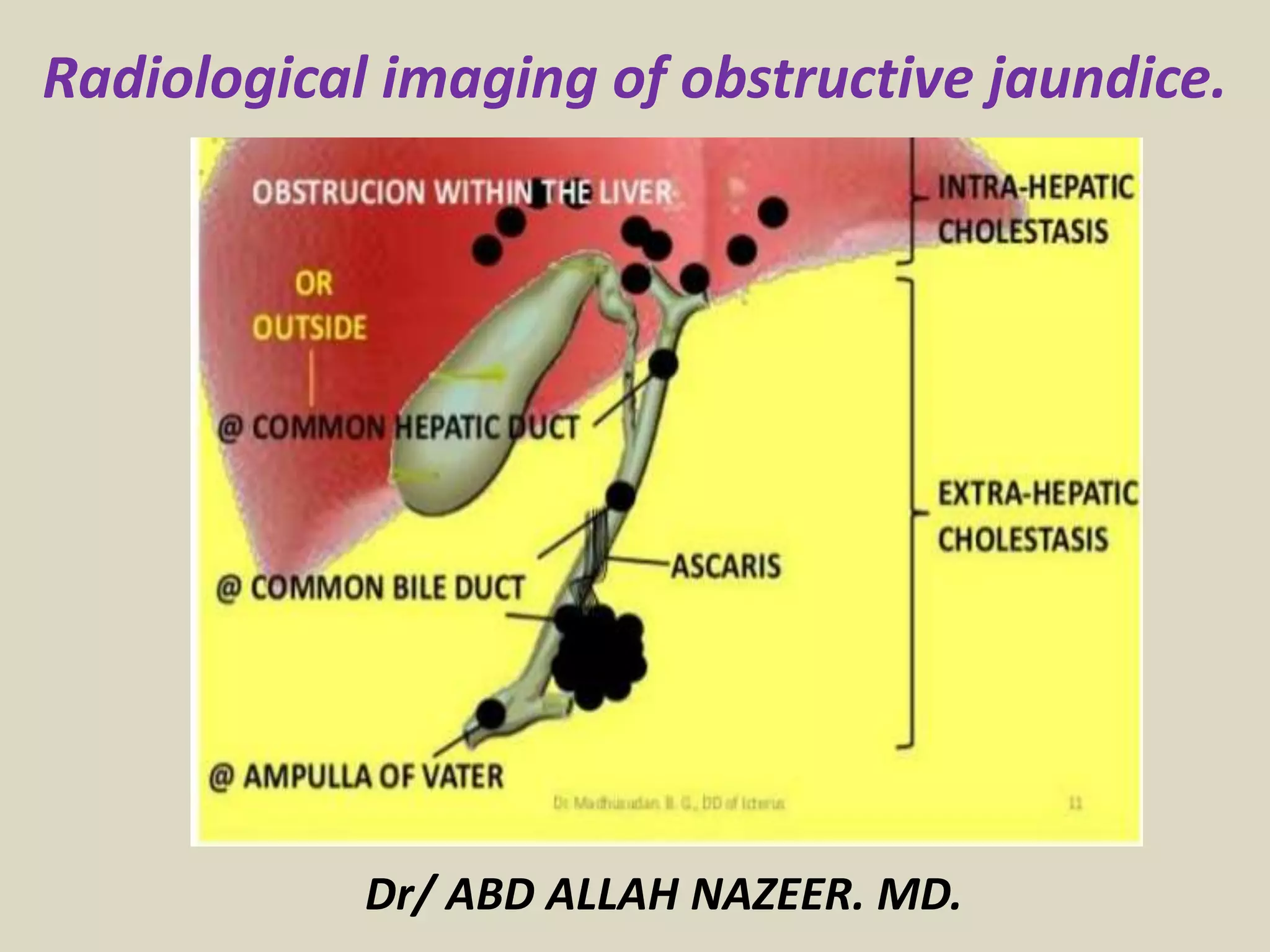
Ultrasonography is the initial test of choice to evaluate obstructive jaundice as it is non-invasive, inexpensive and highly sensitive. It can detect dilated bile ducts suggesting extrahepatic obstruction. MRCP and ERCP provide more detailed imaging of the biliary tree but ERCP allows for therapeutic interventions. Other options include CT, PTC and EUS which provide additional information but have greater risks or limitations. The cause of obstructive jaundice can be benign such as gallstones or malignancies involving the bile ducts, pancreas or gallbladder.
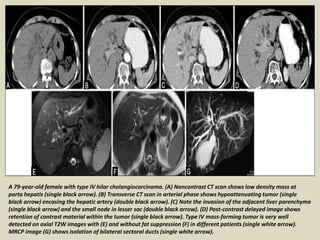
![CT scan has limited value in helping diagnose CBD stones because many
of them are radiolucent and CT scan can only image calcified stones. It is
also less useful in the diagnosis of cholangitis because the findings that
specifically suggest bile duct infection (increased attenuation due to pus,
bile duct wall thickening, and gas) are seen infrequently.
Lastly, CT scan is expensive and involves exposure to radiation, both of
which lessen the routine use CT scans compared to US examinations.
Spiral (helical) CT scan improves biliary tract imaging by providing
several overlapping images in a shorter time than traditional CT scan
and by improving resolution by reducing the presence of respiratory
artifacts. CT cholangiography by the helical CT technique is used most
often to image the biliary system and makes possible visualization of
radiolucent stones and other biliary pathology.[6]
Limitations of helical CT cholangiography include reactions to the
contrast, which are becoming less frequent. Also, as serum bilirubin
levels increase, the ability to visualize the biliary tree diminishes and the
ability to fully delineate tumors decreases. Patients are required to hold
their breath while images are acquired.](https://image.slidesharecdn.com/presentation1-160625210029/85/Presentation1-pptx-radiological-imaging-of-obstructive-jaundice-3-320.jpg)
![Percutaneous transhepatic cholangiogram (PTC) is performed by a
radiologist using fluoroscopic guidance.[7] The liver is punctured to enter
the peripheral intrahepatic bile duct system. An iodine-based contrast
medium is injected into the biliary system and flows through the ducts.
Obstruction can be identified on the fluoroscopic monitor. It is especially
useful for lesions proximal to the common hepatic duct.
The technique is not easy and requires considerable experience. More than
25% of attempts fail (most often when the ducts cannot be well visualized
because they are not dilated, i.e., not obstructed.)
Complications of this procedure include the possibility of allergic reaction
to the contrast medium, peritonitis with possible intraperitoneal
hemorrhage, sepsis, cholangitis, subphrenic abscess, and lung collapse.
Severe complications occur in approximately 3% of cases.
The accuracy of PTC in elucidating the cause and site of obstructive
jaundice is 90-100% for causes within the biliary tract. The biliary tree can
be successfully visualized in 99% of patients with dilated bile ducts and in
40-90% if the bile ducts are not dilated. Still, ERCP is generally preferred,
and PTC is reserved for use if ERCP fails or when altered anatomy precludes
accessing the ampulla.](https://image.slidesharecdn.com/presentation1-160625210029/85/Presentation1-pptx-radiological-imaging-of-obstructive-jaundice-7-320.jpg)
![Endoscopic ultrasound (EUS) combines endoscopy and US to
provide remarkably detailed images of the pancreas and
biliary tree. It uses higher-frequency ultrasonic waves
compared to traditional US (3.5 MHz vs 20 MHz) and allows
diagnostic tissue sampling via EUS-guided fine-needle
aspiration (EUS-FNA).[8]Although endoscopic retrograde
cholangiography is the procedure of choice for biliary
decompression in obstructive jaundice, biliary access is not
always achievable, in which case, interventional endoscopic
ultrasound-guided cholangiography (IEUC) may offer an
alternative to percutaneous transhepatic cholangiography
(PTC). Maranki et al reported their 5-year experience with IEUC
in patients who had unsuccessful treatment with ERCP.The
investigators used either a transgastric-transhepatic or
transenteric-transcholedochal approach to the targeted biliary
duct, then advanced a stent over the wire into the biliary tree.](https://image.slidesharecdn.com/presentation1-160625210029/85/Presentation1-pptx-radiological-imaging-of-obstructive-jaundice-8-320.jpg)