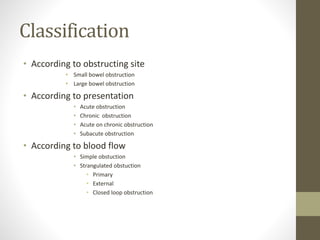
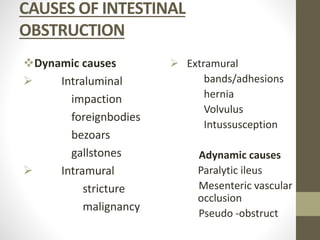
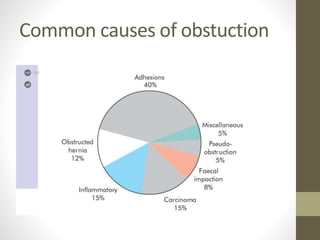
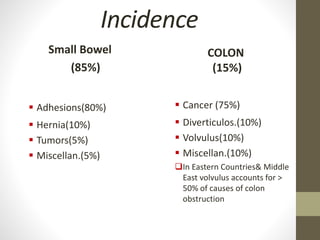
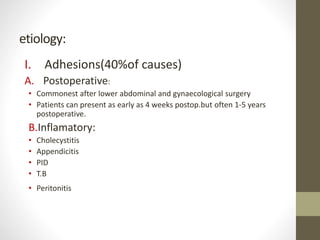
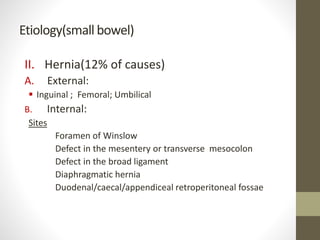
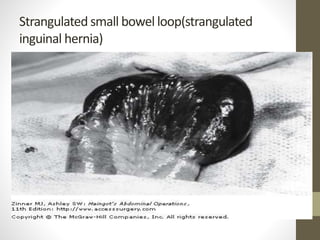
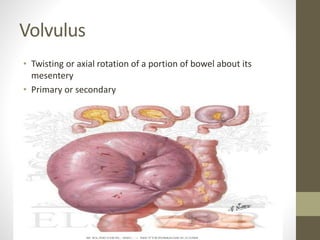
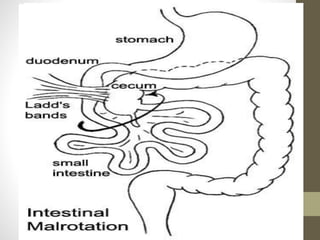
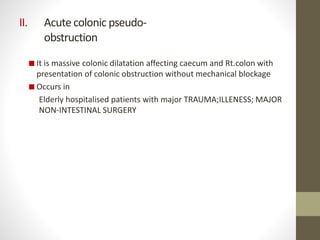
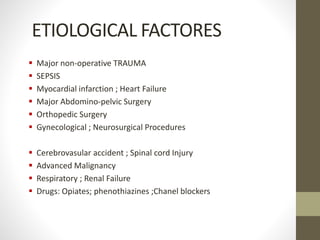
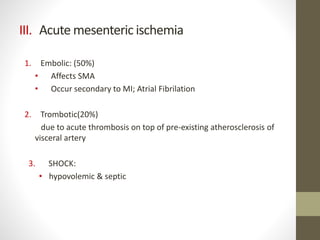
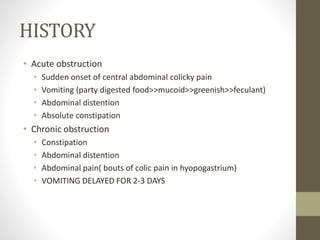
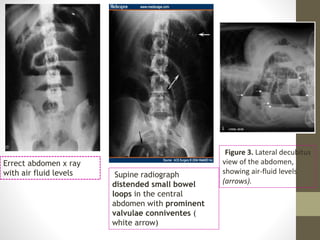
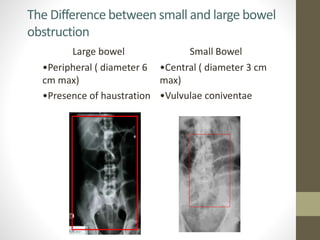
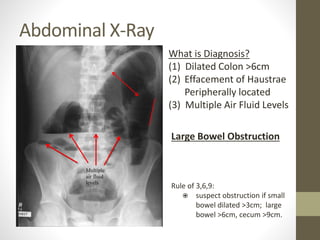
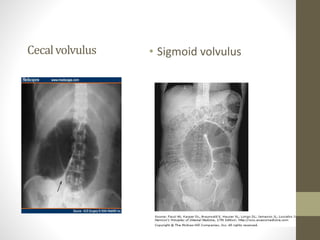
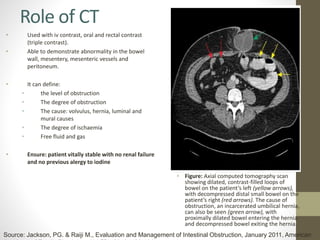
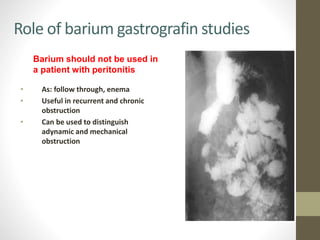
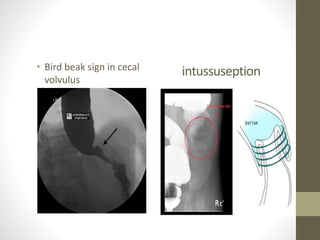
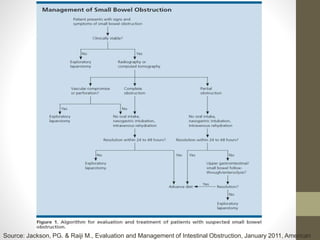
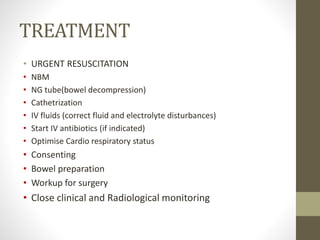
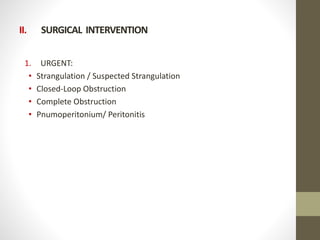
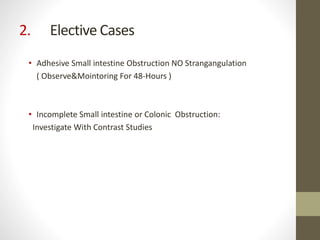
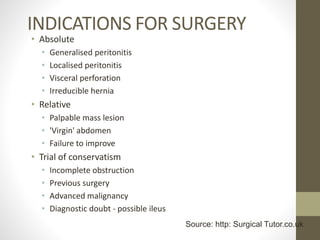
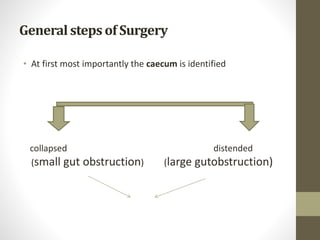
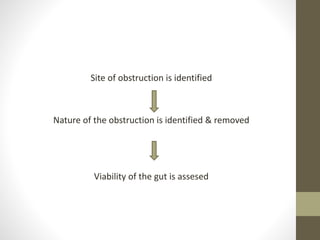
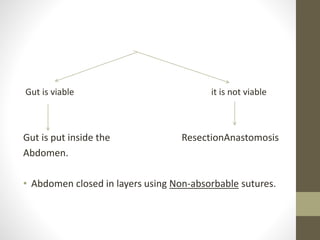
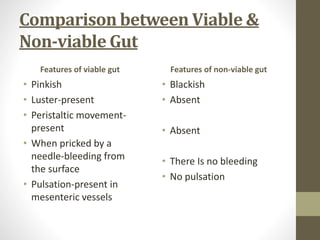
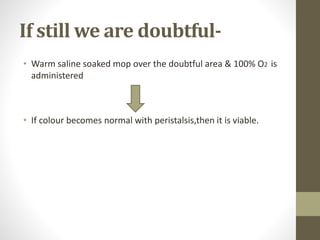
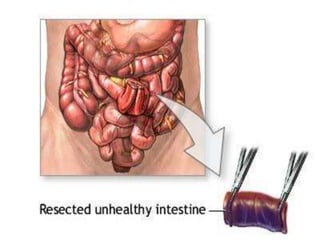
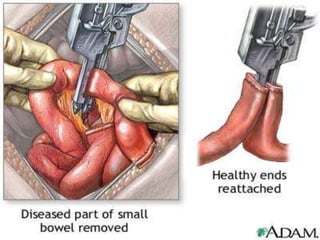
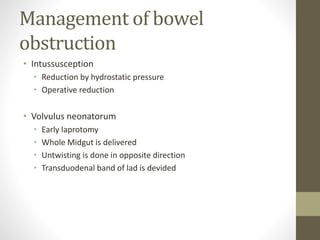
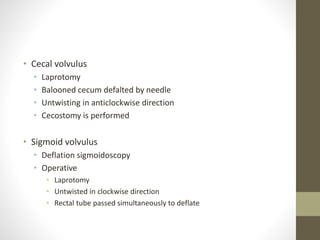
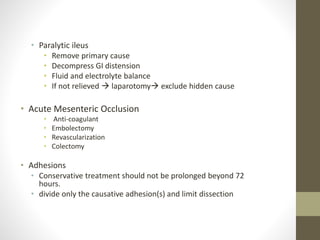
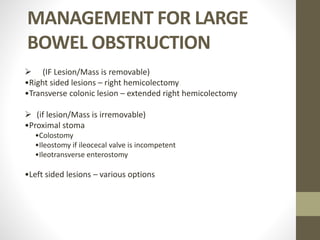
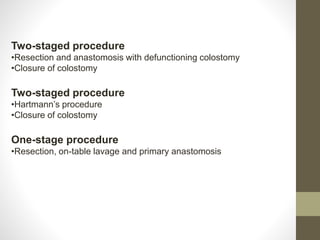
This document discusses intestinal obstruction, including its classification, etiology, causes, symptoms, diagnosis and management. It classifies obstruction by site (small vs large bowel), presentation (acute, chronic, acute on chronic), and blood flow (simple vs strangulated). Common causes are adhesions, hernias, tumors, strictures and volvulus. Diagnosis involves history, exam, labs, imaging like abdominal X-rays and CT scans. Treatment depends on the severity and includes resuscitation, NG decompression, IV fluids, antibiotics if needed, and surgery for severe cases to remove the obstruction. Surgical procedures vary based on the site and nature of the obstruction.