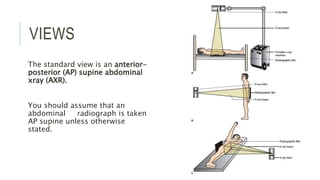
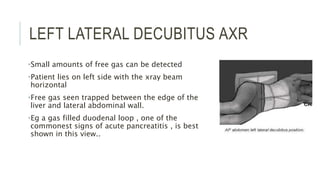
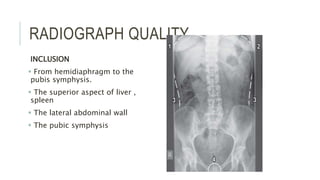
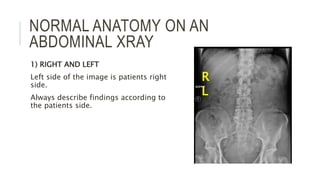
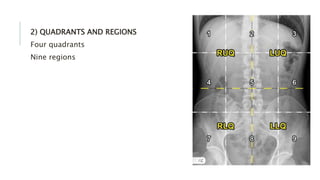
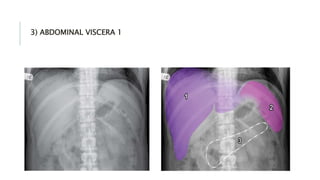
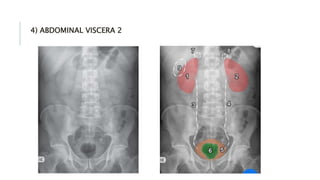
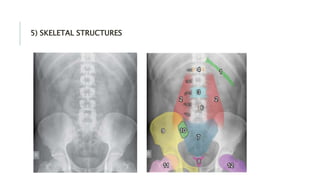
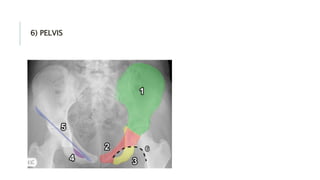
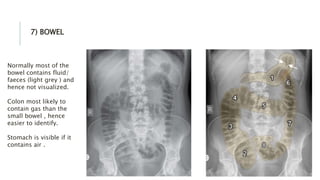
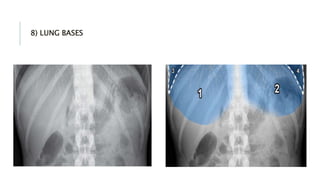
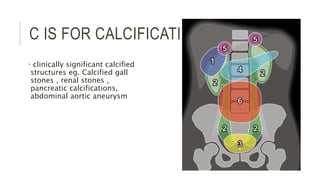
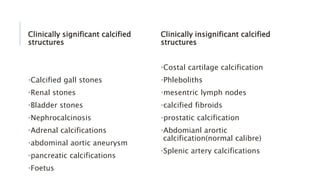
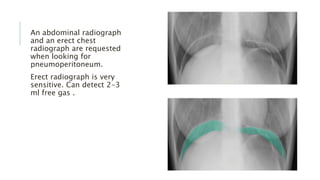
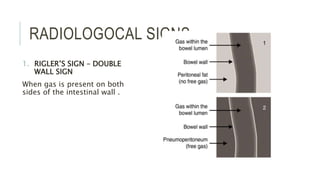
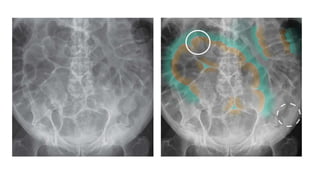
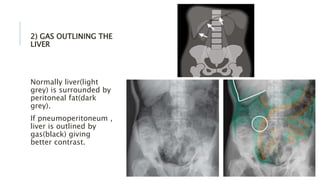
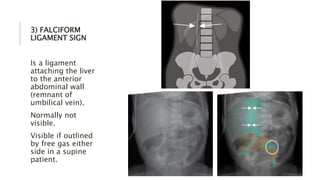
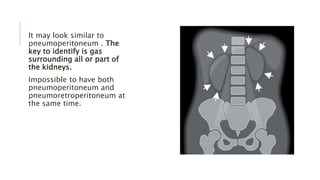
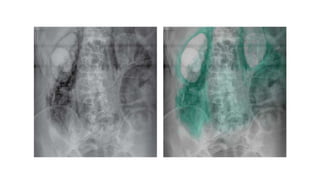
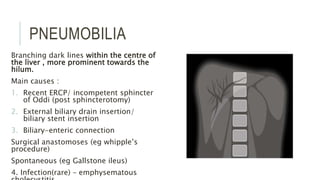
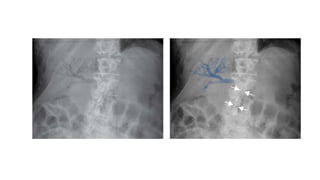
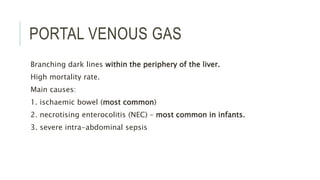
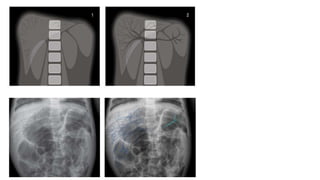
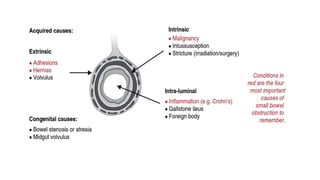
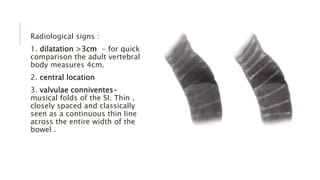
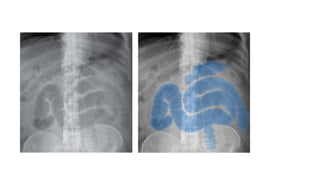
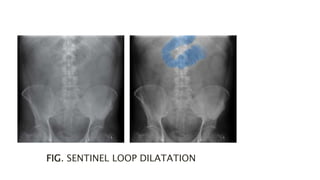
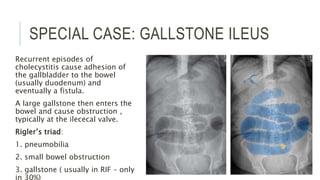
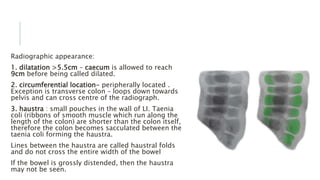
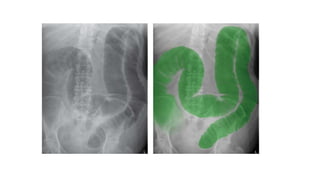
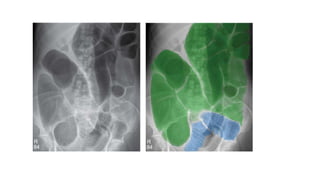
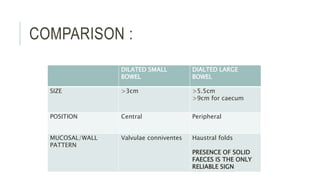
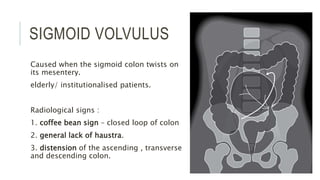
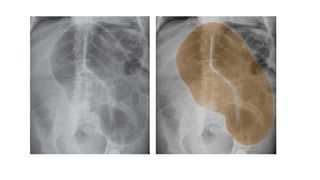
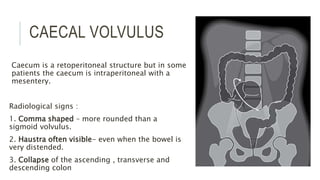
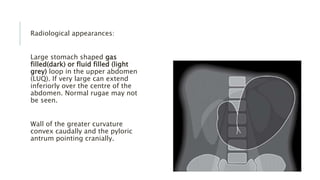
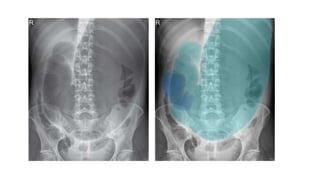
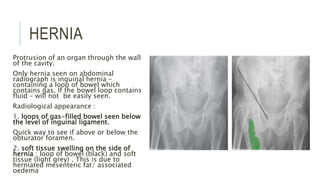
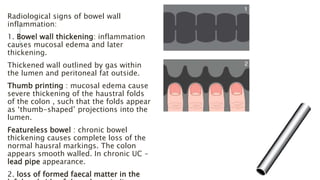
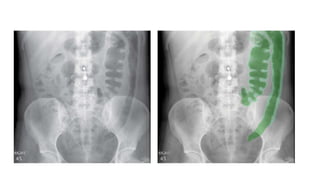
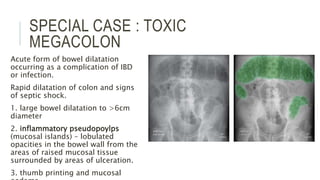
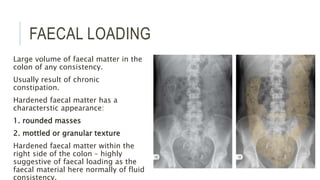
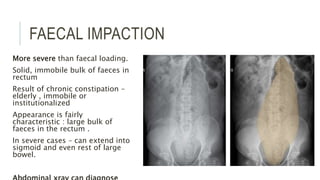
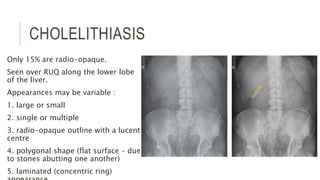
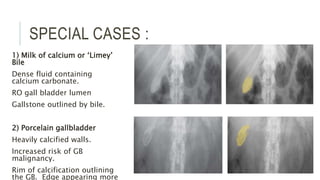
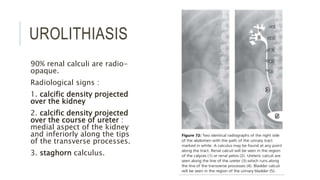
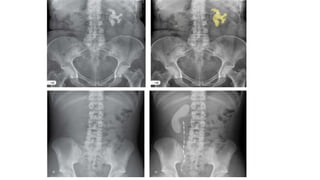
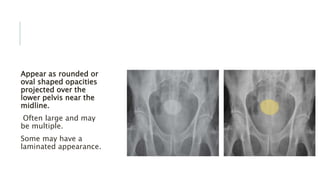
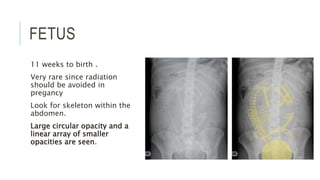
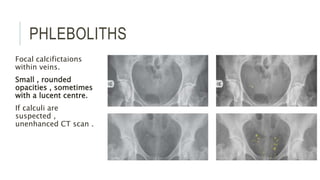
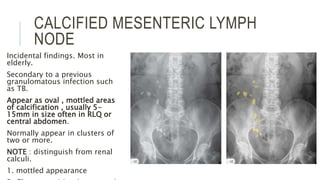
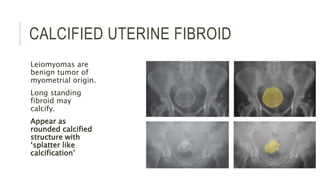
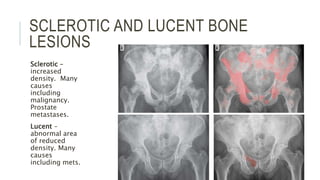
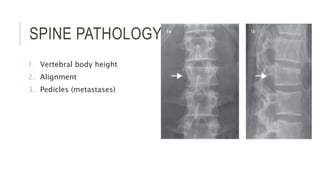
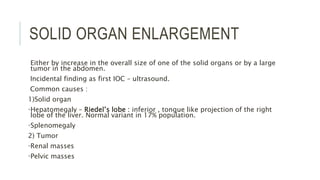
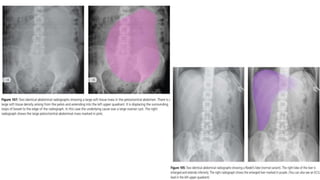
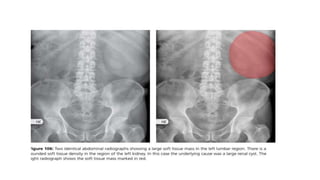
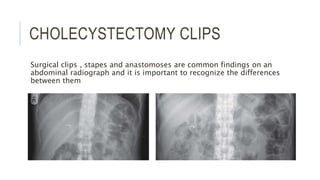
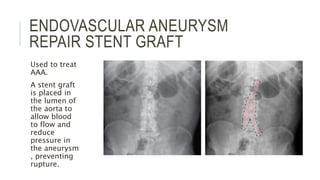
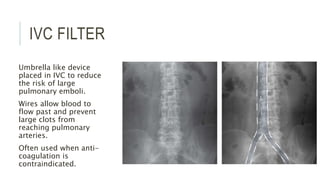
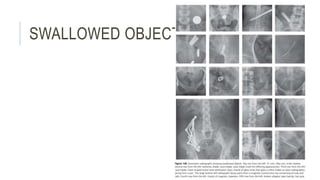
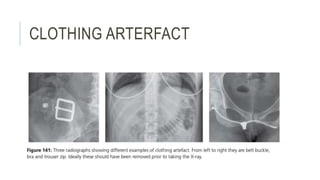
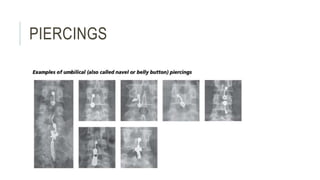
The document provides an extensive overview of abdominal X-ray techniques and interpretations for diagnosing acute abdomen conditions, emphasizing indications, standard views, and key radiological signs. It outlines specific abnormalities such as bowel obstructions, pneumoperitoneum, and faecal loading, along with detailed descriptions of conditions like gallstone ileus and bowel wall inflammation. The summary includes guidance on assessing radiographs through a structured approach, highlighting critical findings and their clinical significance.