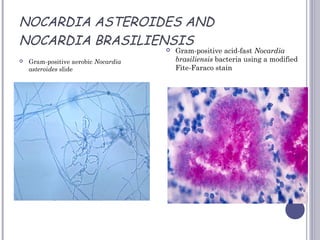
This document discusses Actinomycetes and Nocardia. It describes Actinomycetes as transitional forms between bacteria and fungi that resemble both in certain characteristics. Three medically important genera are mentioned: Actinomyces, Nocardia, and Streptomyces. Actinomycosis is described as a chronic granulomatous infection caused by Actinomyces that presents with indurated swellings and discharge of sulfur granules. Nocardia is described as aerobic, acid-fast, and a cause of cutaneous and systemic infections in immunocompromised individuals. Streptomyces can cause actinomycotic mycetoma, a subcutaneous infection that can penetrate deeper tissues