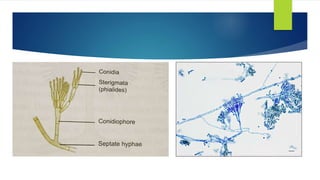
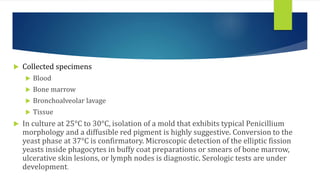
Penicilliosis is an infection caused by Penicillium marneffei that predominantly affects HIV-positive individuals in Southeast Asia. It is characterized by fever, skin lesions, anemia, lymphadenopathy and hepatomegaly. Laboratory diagnosis involves examining specimens such as blood, bone marrow and tissue under a microscope to identify the characteristic yeast and mold forms. Treatment involves antifungal medications such as amphotericin B or oral itraconazole.