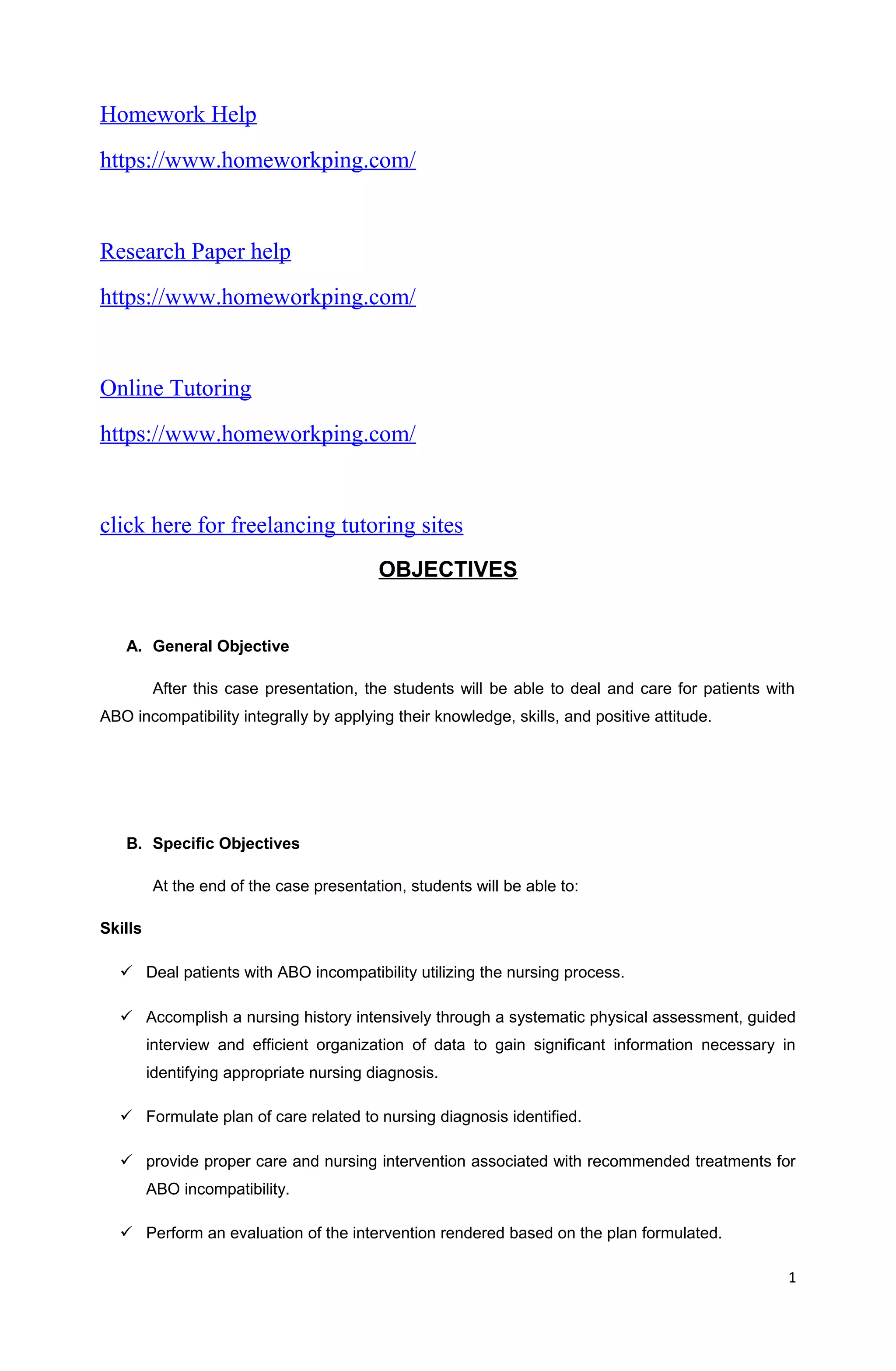
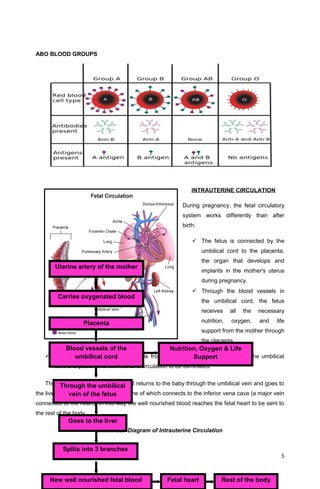
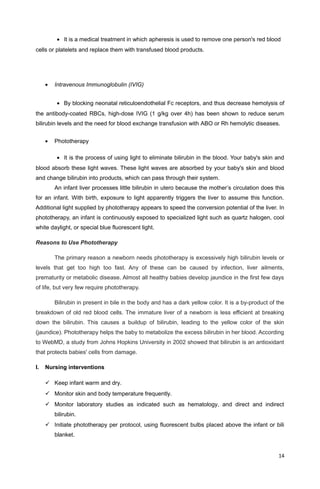
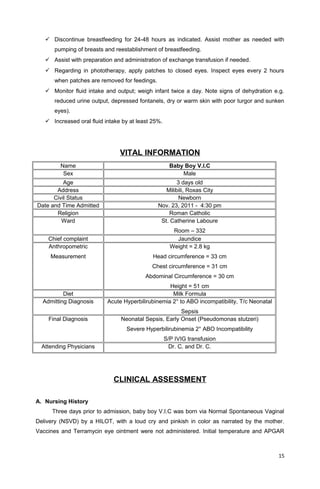
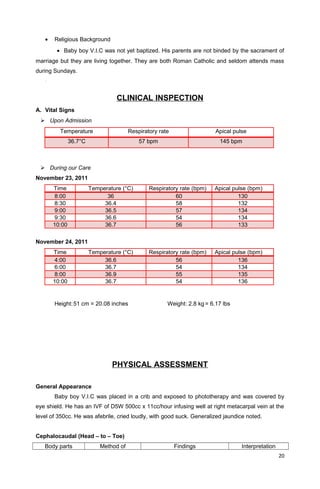
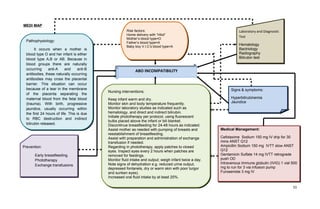
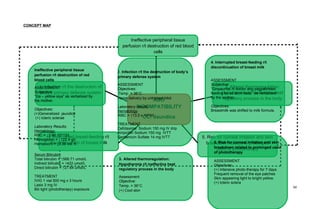
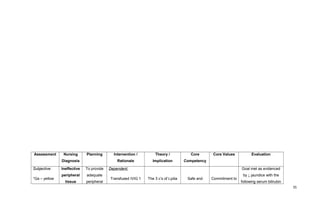
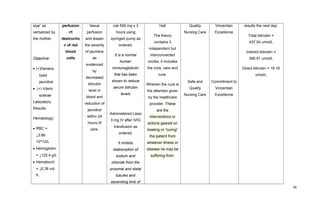
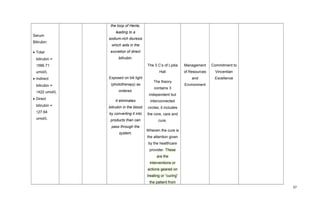
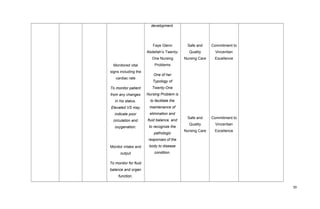
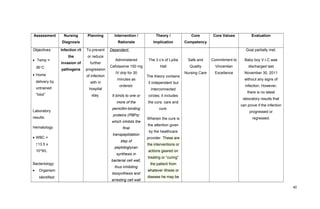
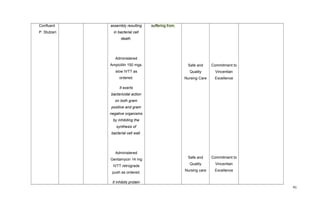
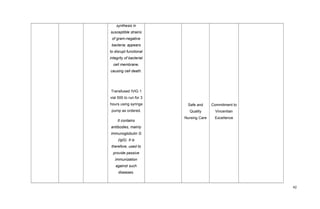
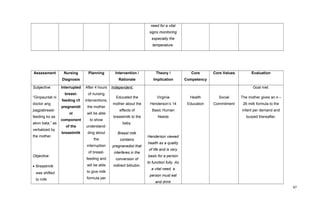
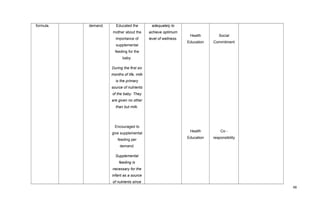
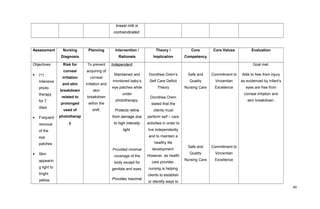
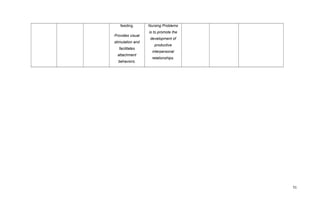
This document provides information about ABO incompatibility and hemolytic disease of the newborn. It begins with an introduction to ABO blood types and compatibility. The causes of ABO incompatibility are described as an immune reaction that occurs when blood from incompatible blood types mix. This can cause hemolysis of the fetus's red blood cells. The document then discusses the anatomy and physiology related to blood groups, bilirubin production and elimination, intrauterine and extrauterine circulation. It provides details on the symptoms, exams, and tests for ABO incompatibility and hemolytic disease of the newborn.