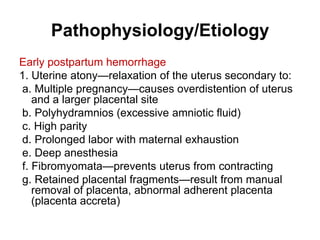
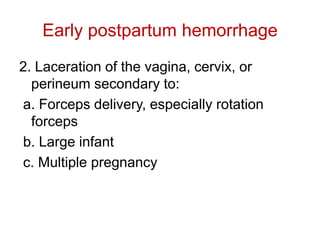
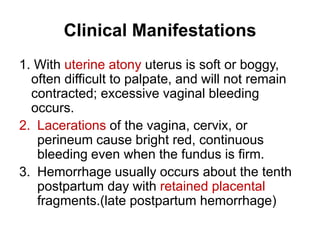
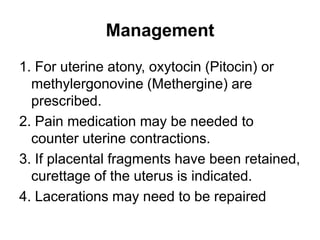
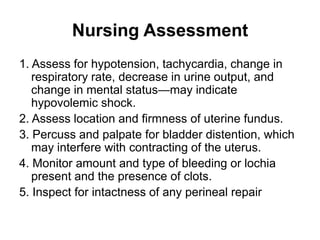
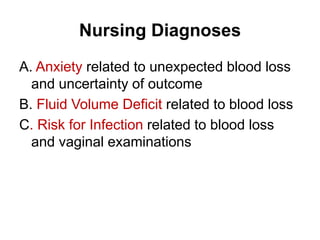
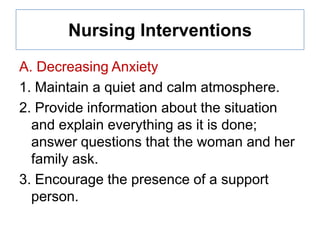
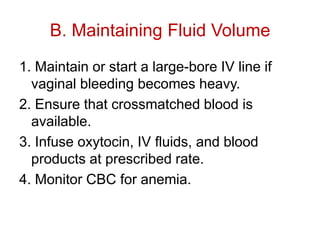
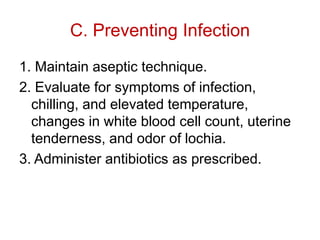
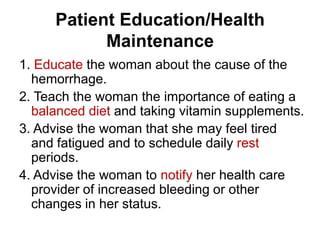
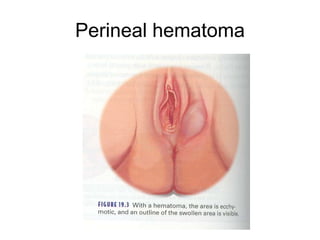
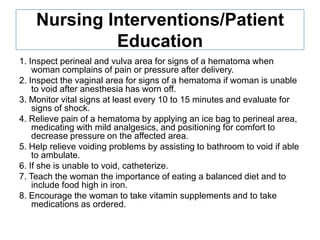
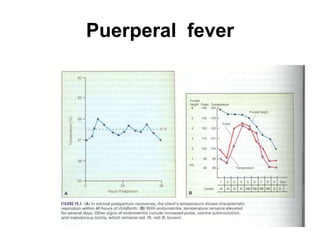
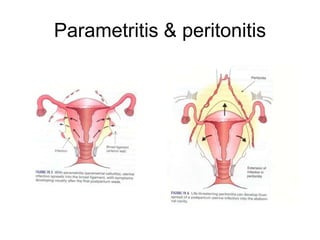
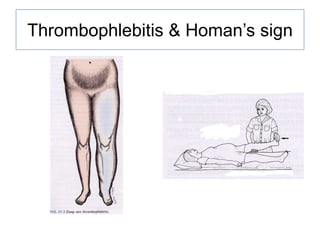
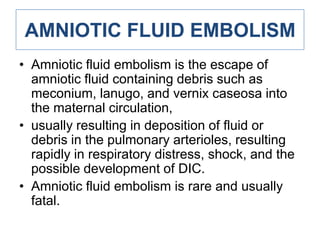
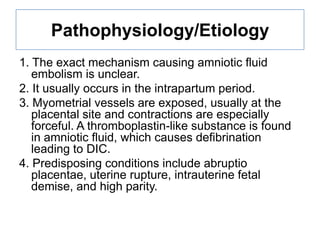
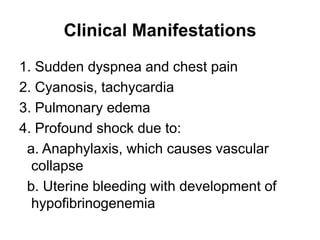
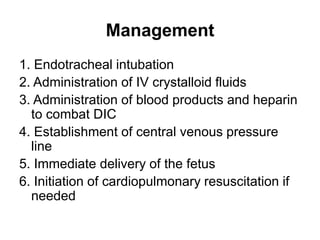
Postpartum hemorrhage and other complications are described. Uterine atony is a common cause of early postpartum hemorrhage. Retained placental fragments can also cause hemorrhage. Clinical manifestations of hemorrhage include hypotension and vaginal bleeding. Management involves oxytocics, IV fluids, blood transfusion, and curettage if needed. Nursing focuses on monitoring for shock, administering treatments, and educating on postpartum care and warning signs. Puerperal infections and hematomas are also risks and are managed with antibiotics, analgesics, and hygiene education. Amniotic fluid embolism is a rare but often fatal complication from amniotic debris entering the mother's