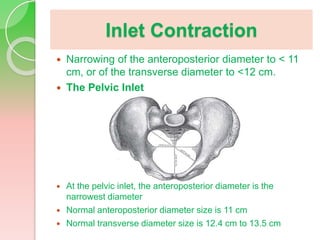
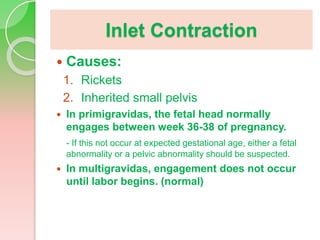
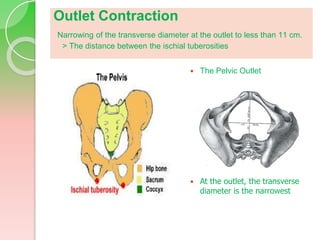
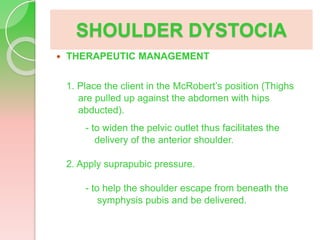
This document discusses several conditions that can cause difficulties during childbirth due to the size relationship between the baby's head and the mother's pelvis, including inlet contraction, outlet contraction, and cephalopelvic disproportion. It describes the normal measurements of the pelvic inlet and outlet, potential causes of each condition, assessment findings, management strategies, and complications. It also covers shoulder dystocia, defining it as when the baby's anterior shoulder gets stuck under the pubic bone after the head is delivered. Risk factors, pathophysiology, assessment findings, and management techniques like McRoberts position and suprapubic pressure are outlined.