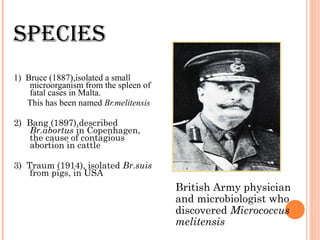
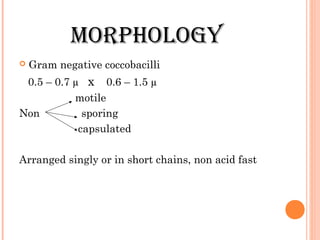
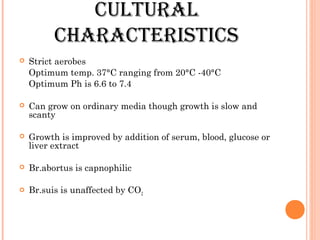
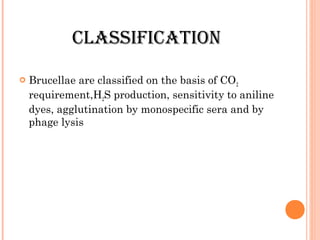
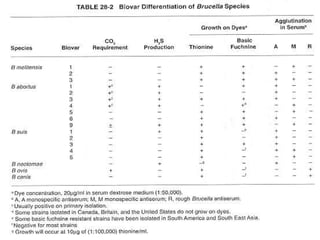
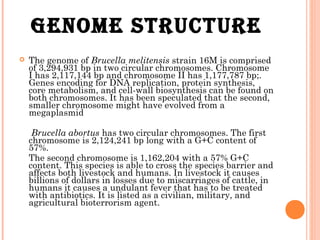
This document provides information on Brucella, the causative agent of brucellosis. It discusses the classification of Brucella as an alpha Proteobacteria. The main Brucella species that infect humans are B. melitensis, B. abortus, and B. suis, which are transmitted through contact with infected animals. The document outlines the morphology, culture characteristics, pathogenicity, diagnosis, treatment and prevention of Brucella infections. Brucellosis is a widespread zoonotic disease that can cause acute or chronic infections in humans.