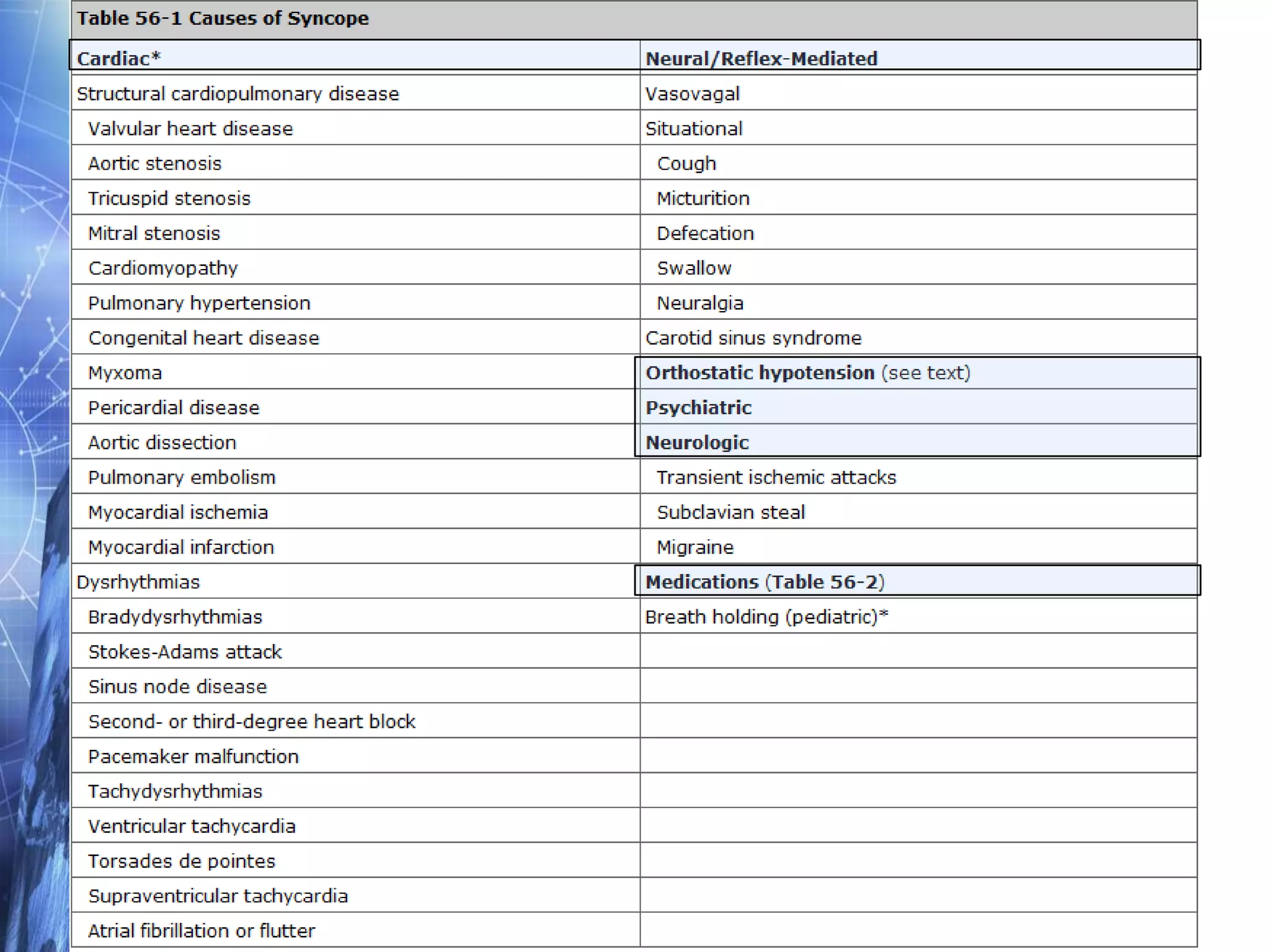
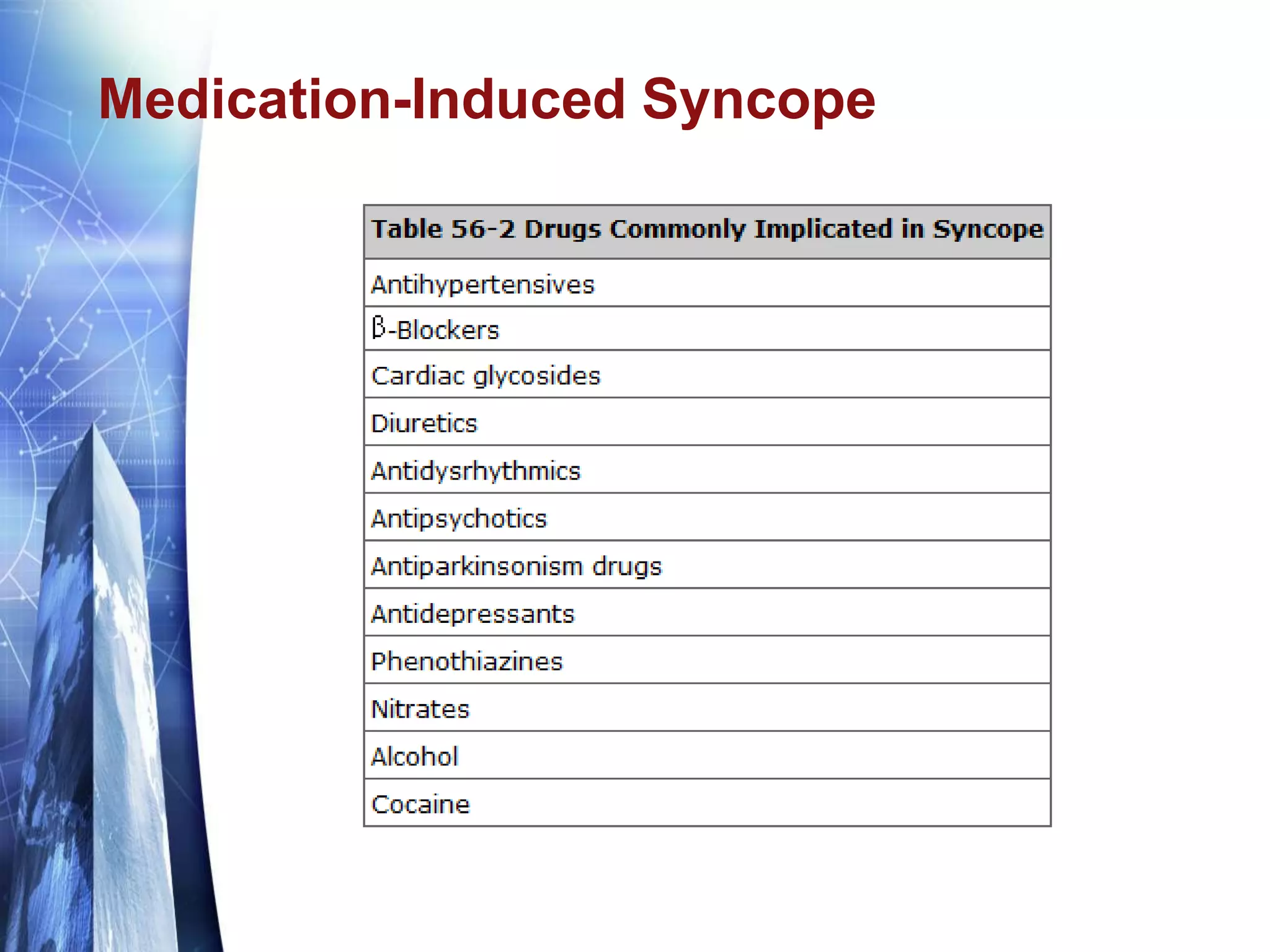
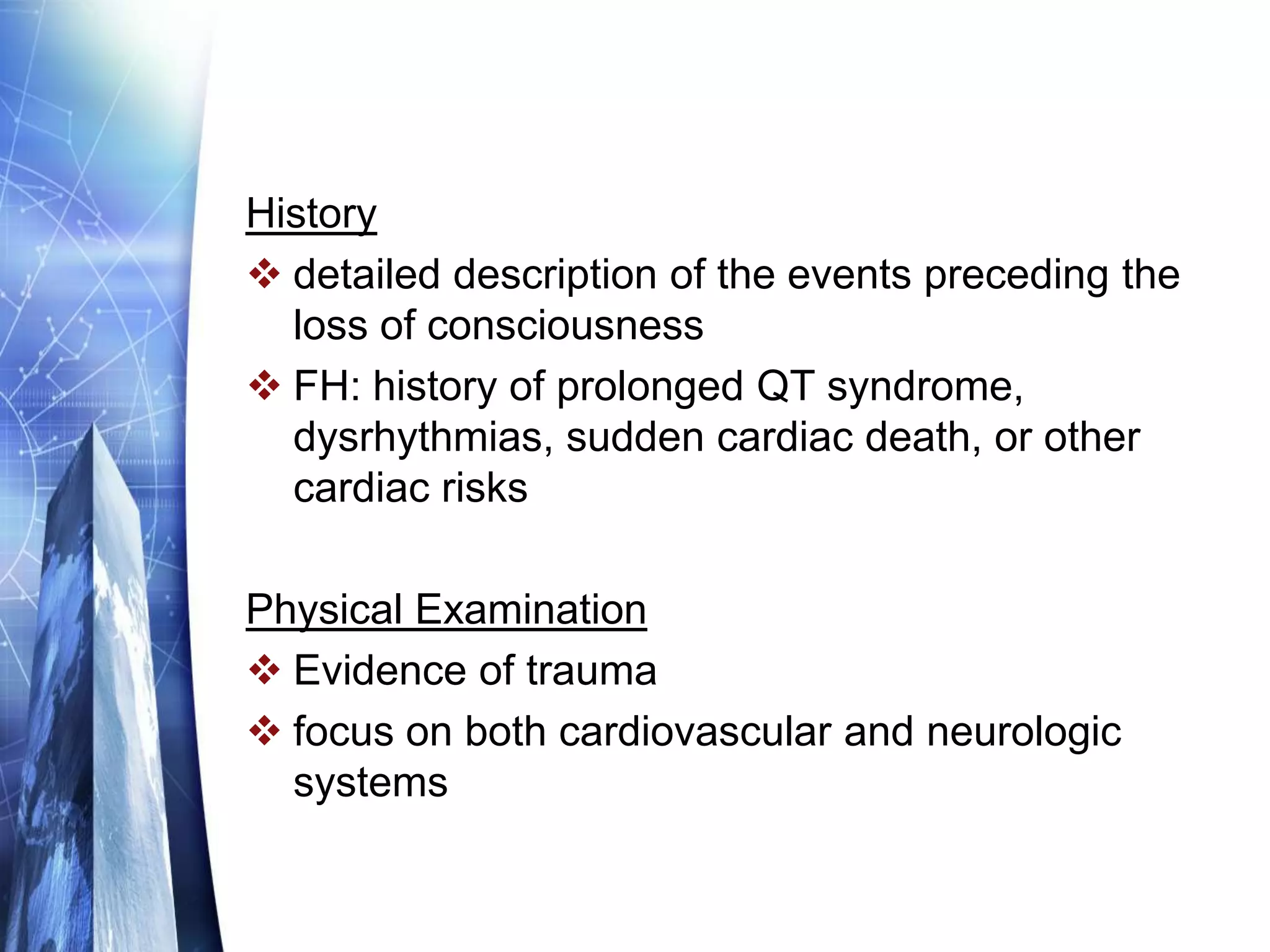
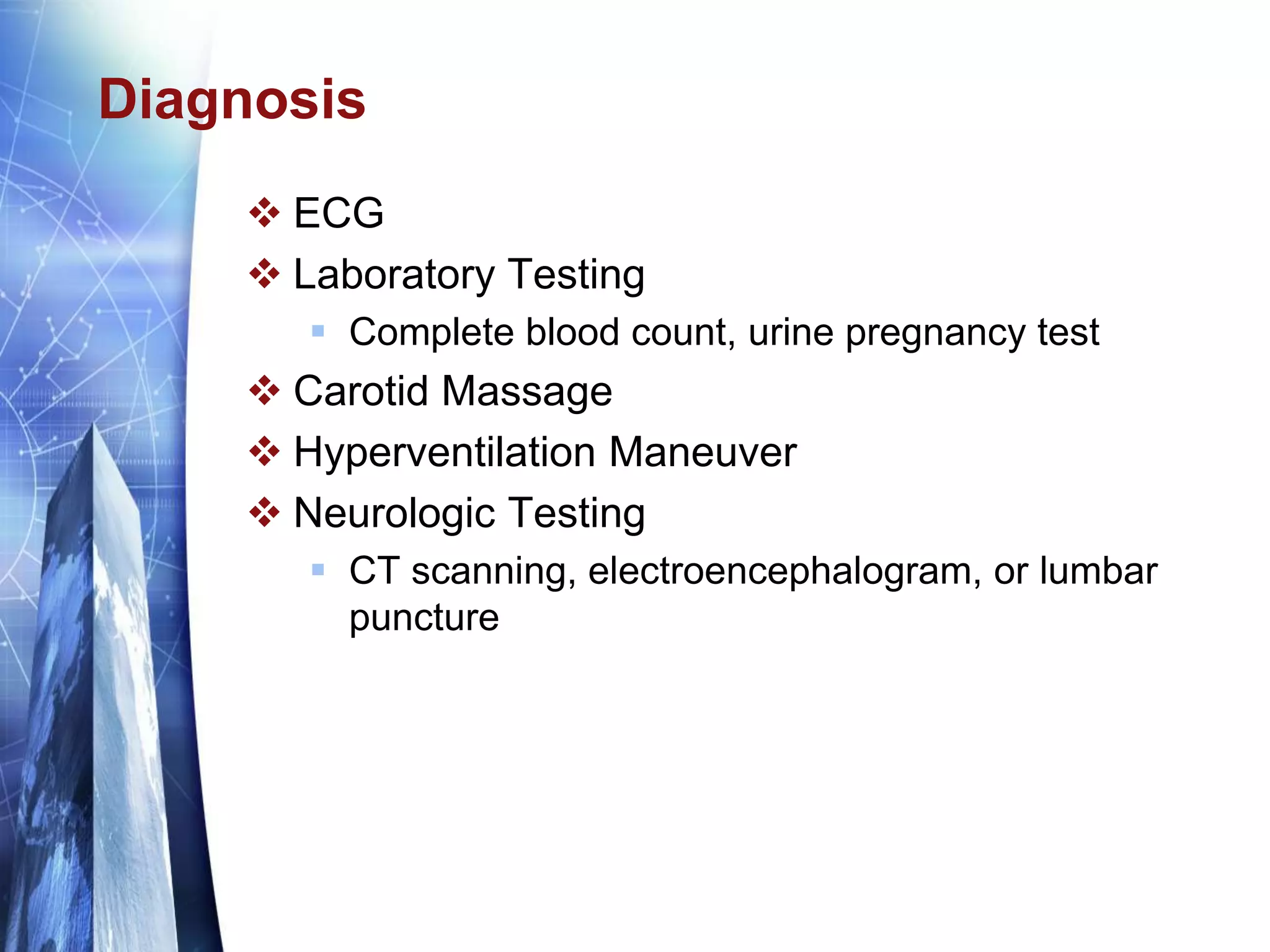
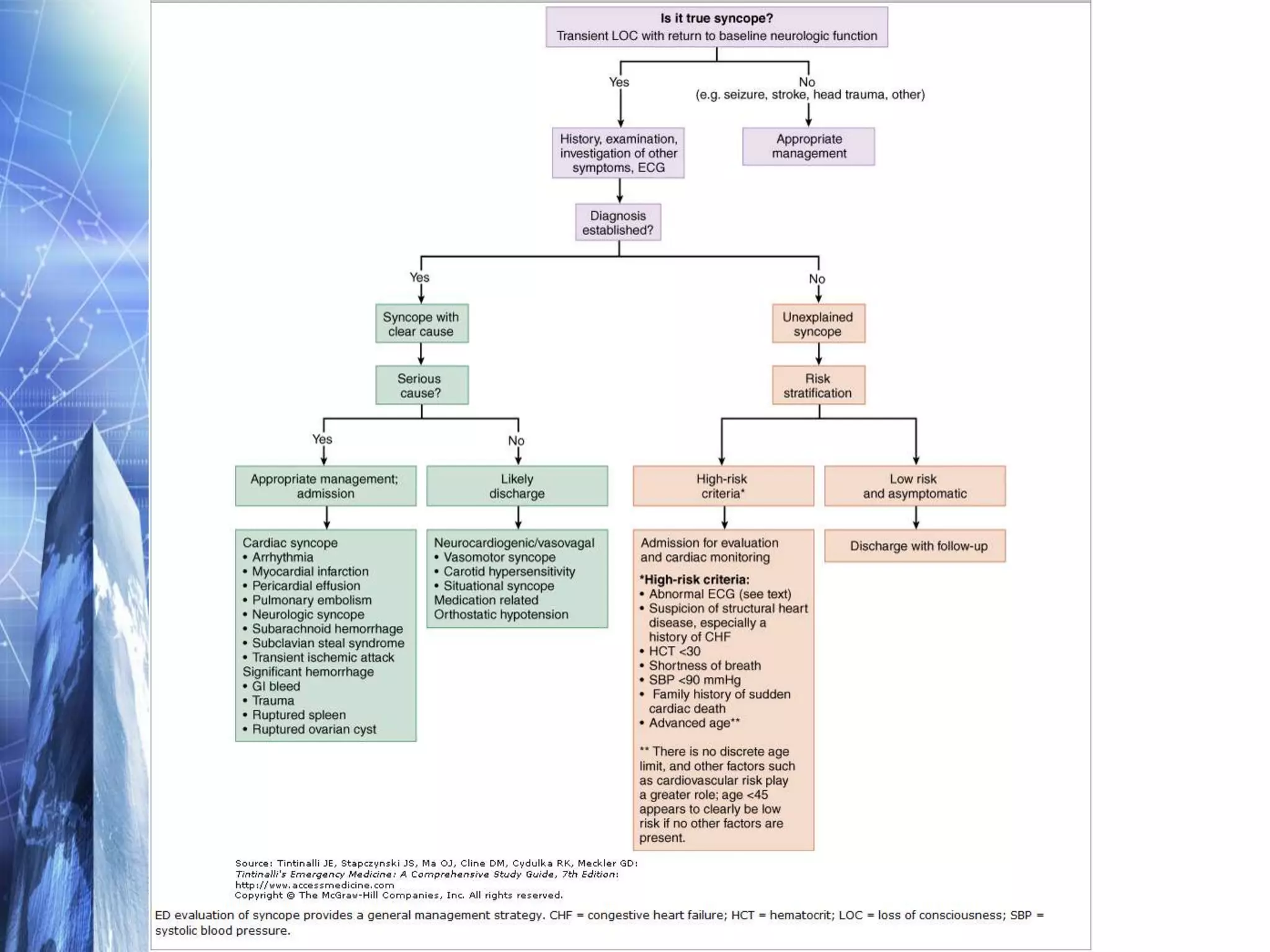
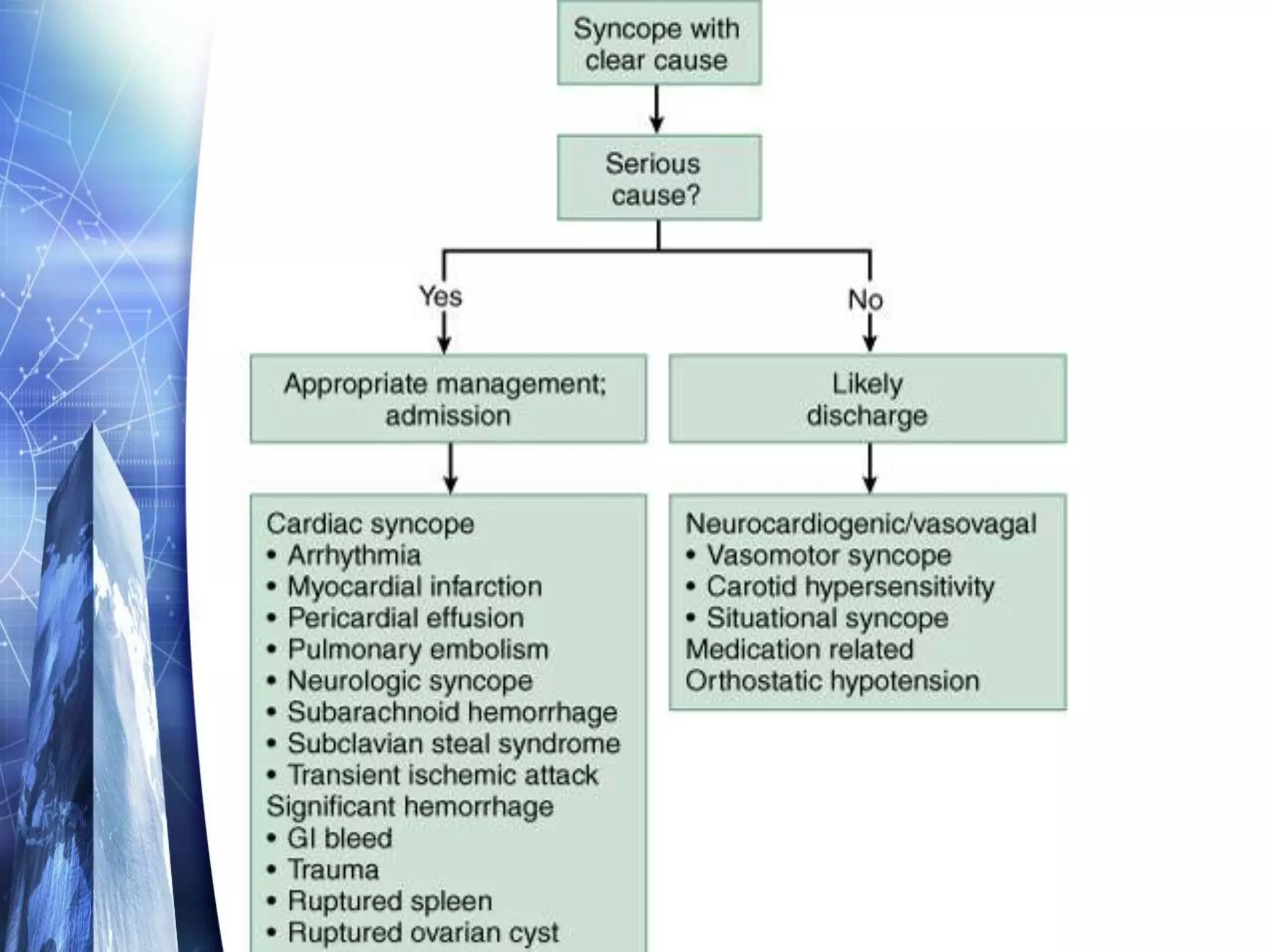
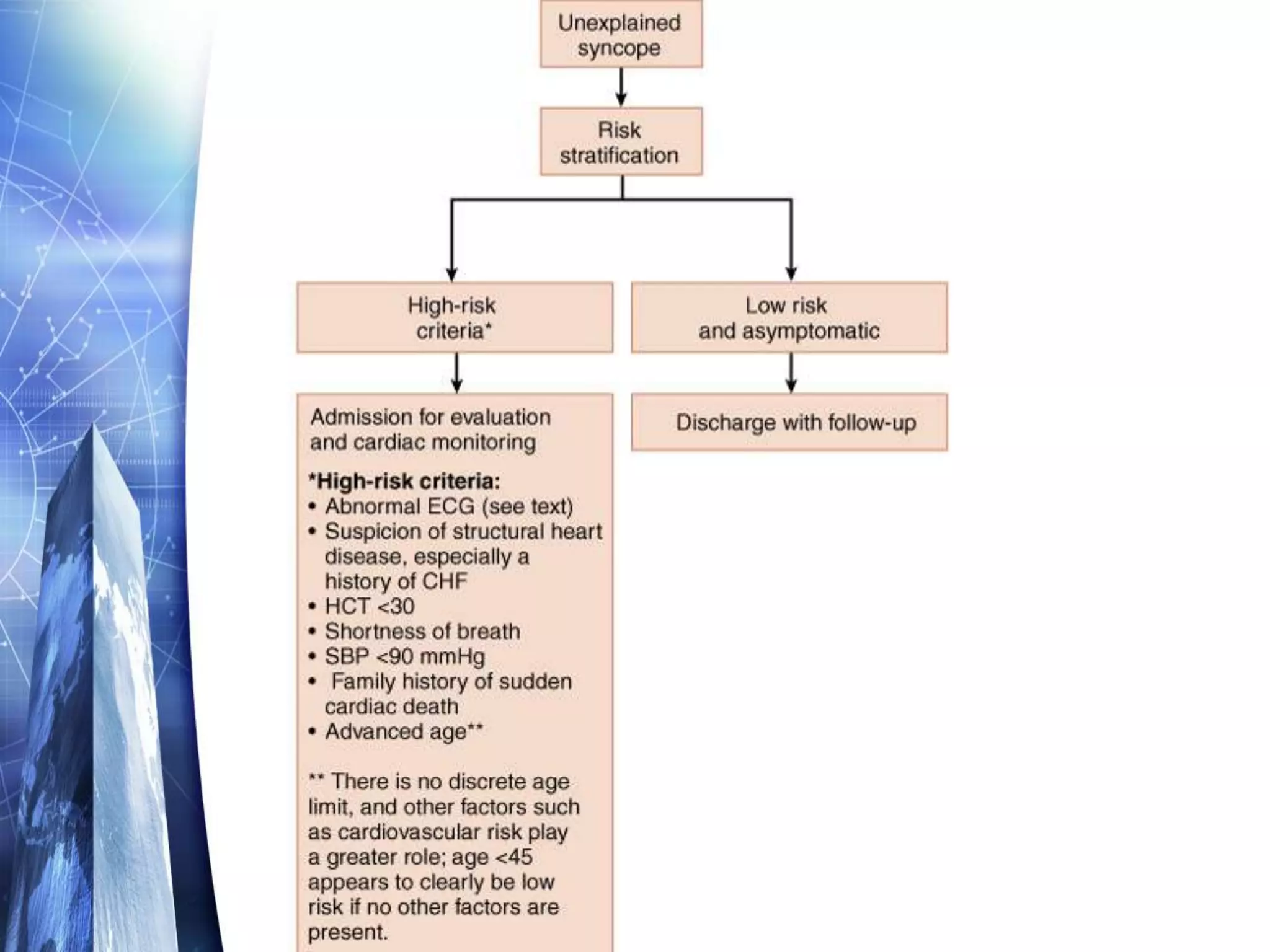
This document discusses syncope, which is a brief loss of consciousness due to decreased blood flow to the brain. It can be caused by cardiac issues like aortic stenosis or arrhythmias, neurological issues like carotid sinus hypersensitivity, orthostatic changes in blood pressure, psychiatric conditions, or certain medications. The evaluation of syncope involves taking a detailed history, performing a physical exam focusing on cardiovascular and neurological systems, doing tests like an ECG, labs, and tilt table testing, and considering imaging if needed to diagnose the underlying cause. Treatment depends on the identified cause but the goal is to prevent future episodes.