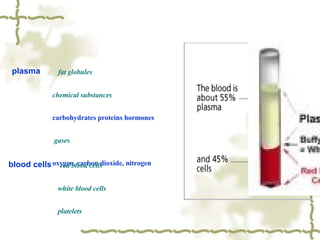
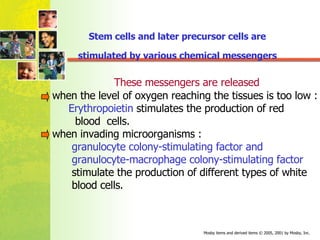
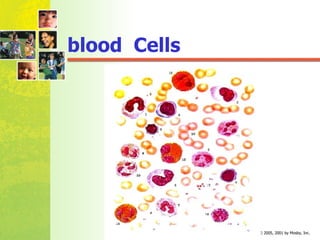
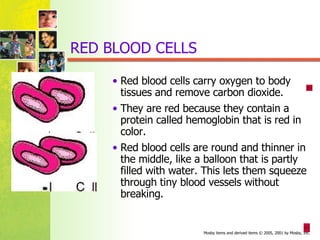
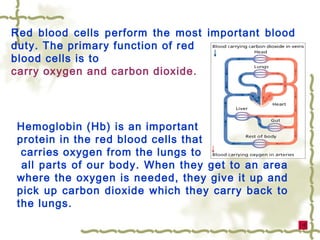
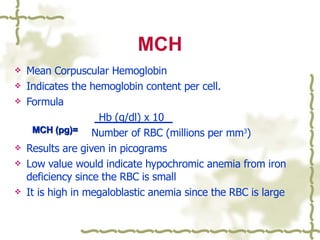
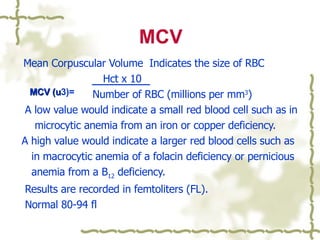
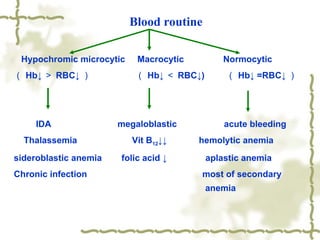
The document discusses features of blood in children, including plasma, blood cells, and hematopoiesis. Hematopoiesis is the process of blood cell production, which occurs in the mesoblast, liver, spleen, and bone marrow during fetal development and shifts to primarily the bone marrow after birth. The document provides details on red blood cells, white blood cells, platelets, and blood volume in children at different ages. It also discusses anemia and the classification of anemia severity based on hemoglobin and red blood cell counts.