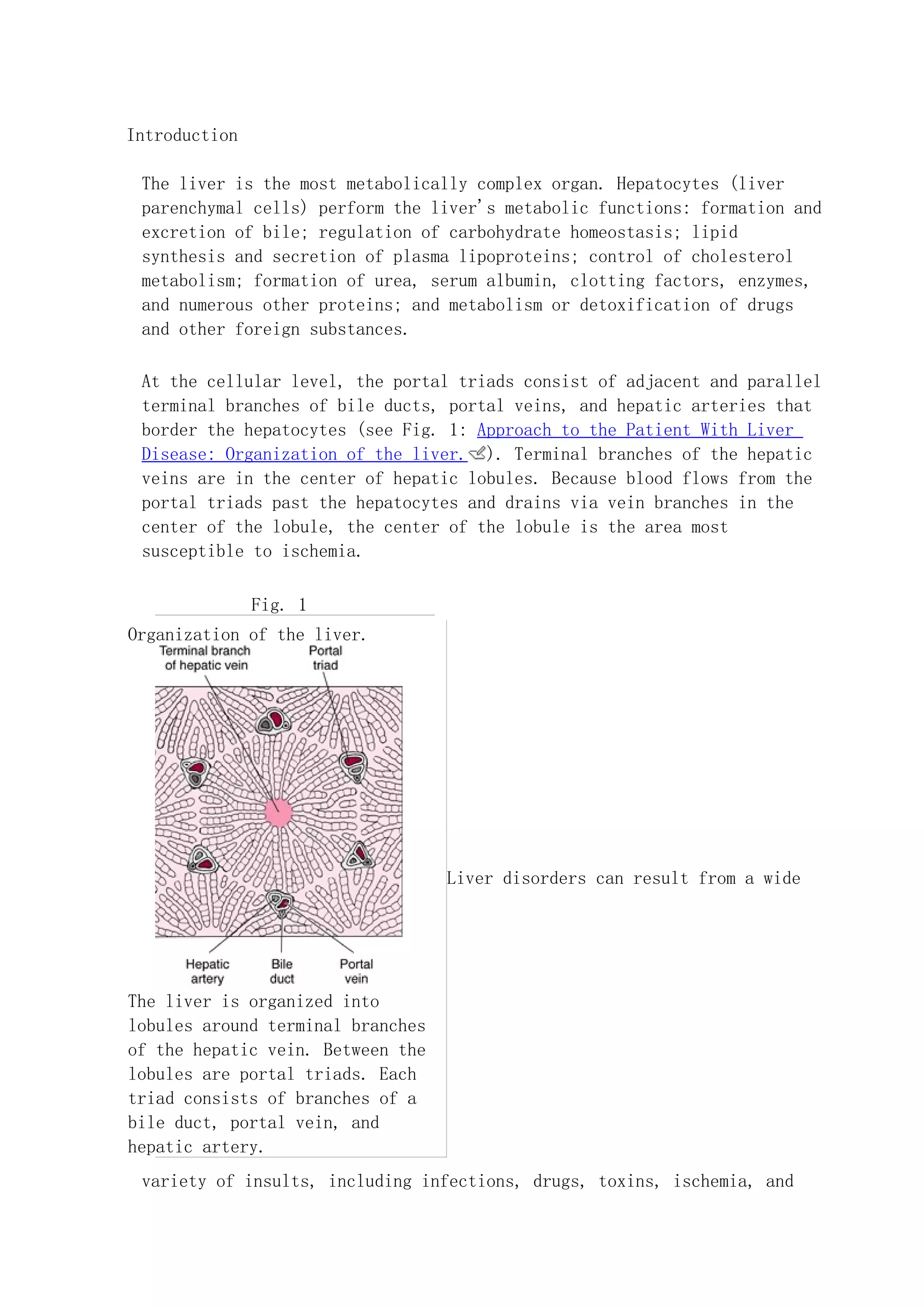
The liver is organized into lobules centered around branches of the hepatic vein. Between the lobules are portal triads containing branches of the bile duct, portal vein, and hepatic artery. Hepatocytes within the lobules perform many metabolic functions. Liver disorders can result from infections, drugs, toxins, ischemia, autoimmune issues, or postoperative issues. Postoperative liver dysfunction may occur without preexisting liver disease due to ischemia or anesthesia and usually resolves, but can worsen preexisting conditions like hepatitis.